Articles
- Page Path
- HOME > Restor Dent Endod > Volume 28(6); 2003 > Article
- Original Article The influence of epinephrine concentration in local anesthetics on pulpal and gingival blood flows
- Jae-Sang Lee, Sung-Kyo Kim
-
2003;28(6):-484.
DOI: https://doi.org/10.5395/JKACD.2003.28.6.475
Published online: November 30, 2003
Department of Conservative Dentistry, School of Dentistry, Kyungpook National University, Korea.
- Corresponding author: Sung-Kyo Kim. Department of Conservative Dentistry, School of Dentistry, Kyungpook National University, 188-1, 2-Ga, Samdeok-Dong, Jung-Gu, Daegu 700-412, Republic of Korea. Tel: 053-420-5935, Fax: 053-426-8958, skykim@knu.ac.kr
Copyright © 2003 Korean Academy of Conservative Dentistry
- 2,197 Views
- 9 Download
- 3 Crossref
I. INTRODUCTION
Local anesthetics with vasoconstrictor have been widely used in dentistry for the control of pain and also for the control of hemorrhage1). Surgical anesthesia has been achieved more than twice as frequently with a local anesthetic solution containing vasoconstrictor as one without vasoconstrictor2), and it has been recommended those local anesthetic solutions containing vasoconstrictor should be used routinely for patient comfort1).
The most common vasoconstrictor is epinephrine, which has been used in concentrations from 1:50,000 to 1:300,000 to produce several beneficial effects: decrease in plasma concentration of local anesthetic, increase in duration and quality of anesthesia, reduction in amount of anesthetic needed, and hemostasis during surgical procedures3). For these benefits, local anesthetics with epinephrine is generally recommended in clinical dentistry.
Local anesthetics are used not only in conventional endodontic treatment to control pain during pulp extirpation but also in surgical endodontic treatment to control hemorrhage. For the control of hemorrhage, relatively higher concentration of epinephrine, i.e. 1:50,000, is used in surgical endodontics in conjunction with local anesthetics than in nonsurgical endodontics which usually uses epinephrine concentration of 1:100,000. Because bleeding occurs through the gingivomucosal flap reflection and bony cavity preparation, epinephrine induced-vasoconstriction is the first method of hemostasis in the endodontic surgery4-6).
Pulpal circulation and its regulation play an important role in inflammatory processes and pulpal pathophysiology7,8). Since new oxygen is supplied and waste product is removed through the blood circulation, epinephrine induced-blood flow decrease may adversely exert harmful effects on the metabolism of any tissue7). Because pulp represents a terminal circulation, prolonged vasoconstriction may more readily damage the pulp than vasoconstriction of other areas, such as the gingiva, which has more collateral circulation.
For the use of epinephrine in local anesthetics, we need to understand the effect of its concentration on the pulpal and gingival blood flow (GBF), and their relation to pulpal numbness. Even though some papers were published concerning pulpal blood flow (PBF) changes induced by local anesthetics with epinephrine, the influence of epinephrine concentration on the PBF and GBF has been rarely studied.
The purpose of the study was to evaluate the influence of epinephrine concentration on the PBF and GBF, and their relation to pulpal numbness induced by local anesthesia by simultaneous recording of both blood flows and pulpal response to electrical stimulus.
II. MATERIALS AND METHODS
Maxillary central incisors of ten volunteers aged 24 to 27 (7 males, 3 females) were selected. Informed consent was obtained from all subjects involved in the study. The following criteria for the maxillary left central incisors were used in selecting the volunteers: no restorations, no tooth discoloration or caries, normal response to both thermal and electrical pulp testing (EPT), no traumatic or orthodontic treated history and normal periapical radiographic finding.
Stabilizing splints were fabricated for each volunteer. After impressions were taken on the upper anterior region, stone casts were made. With an opaque vinyl polysiloxane impression putty (Exafine, GC Corp., Tokyo, Japan), stabilizing splints were fabricated from the cast models for the upper anterior area. Three holes were made through the splint for each tooth. A cervical hole was made on the labial side at approximately 3 to 4 mm from the gingival margin for pulpal probe9); a gingival hole was on the labial side at 3 mm apical to the gingival margin for gingival probe; and an incisal hole was made to reveal the tip of the tooth so that electric pulp testing could be carried out without removing the splint. The position of cervical hole was selected to avoid any potential reflective interference of the signal from the GBF. The splint stabilized the probes against the buccal surfaces of the central incisors minimizing movement artifacts and allowed correct repositioning of the probes.
For the measurement of PBF and GBF, a laser Doppler flowmeter (Periflux 4001, Perimed Co., Stockholm, Sweden) was used. It projects a low power laser light of 780 nm in wavelength and maximum power output of 1 mW. For the measurement of PBF, a dental probe (PF416, Perimed Co., Stockholm, Sweden) of 1.6 mm in diameter and 0.25 mm fiber separation was used toward the labial surface of the crown. For the measurement of GBF, a standard probe (PF408, Perimed Co., Stockholm, Sweden) of 6.0 mm in diameter and 0.25 mm fiber separation was used toward the labial attached gingiva. For the electric pulp testing, a Digitest (Parkell Inc., Farmingdale NY, U.S.A.) was used toward the incisal third of the facial surface of the crown. The laser Doppler flowmetry was calibrated by means of a Motility Standard (Perimed Co., Stockholm, Sweden) before use.
Three different concentrations of epinephrine were used: no epinephrine, 1:100,000, and 1:50,000 epinephrine. 2% plain lidocaine without epinephrine (Kwang Myung Lidocaine, Kwang Myung, Kyunggi-do, Korea) was used as a control in one subject. 2% lidocaine with 1:50,000 epinephrine (AstraPak, Astra USA Inc., Westborough MA, U.S.A.) and 2% lidocaine with 1:100,000 epinephrine (Kwang Myung lidocaine, Kwang Myung, Kyunggi-do, Korea) were used on each subject. Buccal infiltrations were given with a 27-gauge needle placed in the submucosa over the estimated position of the root apex. After aspiration test to avoid accidental intravascular injection before anesthetic administration, 0.9 ml of anesthetic solution, a half carpule, was administered over 30 sec period in each subject.
A data analysis program (PeriSoft, Perimed Co., Stockholm, Sweden) was used to collect and analyze the blood flow signal from the laser Doppler flowmeter. Before experiment, each volunteer was instructed to avoid chewing or moving the mandible during the experiment to minimize movement artifacts. Variables such as stress, external light sources, body position and physiological status of the cardiovascular system were controlled as much as possible, as these could affect blood flow10).
The splint and the two probes were placed and connected to the laser Doppler flowmeter that was connected to a computer. A stable laser Doppler signal 10 min before injection was defined as the baseline value, and the maximum deviation after each administration was used as the experimental value. EPT was also done three times at 1-minute interval to determine an average baseline value. Electrical contact was made with the teeth using electric gel.
After giving the local anesthetics, PBF and GBF were recorded simultaneously and continuously for 70 min. Threshold values to the EPT were recorded manually at 1, 5, 10, 15, 20, 25, 40, 55, and 70 min. Pulpal numbness was considered achieved when the subject gave no response to the maximum output (64 machine units) of the pulp tester. Pulpal numbness was achieved in the all subjects.
The recordings of blood flows were downloaded to a personal computer and the mean percentage of blood flow before and after injection were calculated compared to the baseline value at each time intervals. All numerical data in the text and tables are expressed as percentage change from baseline value and mean SEM. The paired variables of control and experimental data were compared by paired t-test, Wilcoxon's signed rank test, Duncan's multiple range test, and Fisher's exact test. Differences with p<0.05 were considered statistically significant.
III. RESULTS
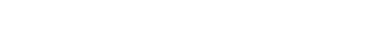
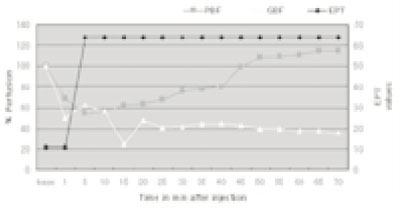
Typical strip-chart recordings of PBF and GBF in response to infiltrative injection of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine are presented in Figures. 1 and 2, and their flow changes are expressed graphically in conjunction with the EPT value in Figures 3 and 4.
When recording baseline value of PBF and GBF before injection of anesthetics, it was possible to establish the pulsatile form of the blood flow reading and obtain a mean value of the information displayed on the screen. When 2% plain lidocaine was injected without epinephrine as a control, PBF was 118.9±2.17% and GBF was 99.66±4.95% of the baseline value. The PBF showed a slight increase but GBF change was not significant from the baseline values (p>0.05).
After administration of 2% lidocaine with 1:100,000 epinephrine, PBF was decreased to 53.36 ±2.39% and GBF was decreased to 18.47±4.88% of the baseline value (Fig. 5). When 2% lidocaine with 1:50,000 epinephrine was administered, PBF was decreased to 43.14±4.76% and GBF was decreased to 17.79±5.07% of the baseline value (Fig. 5). These changes both in the PBF and GBF are significant from the baseline values (p<0.05). GBF was significantly more decreased than PBF in both epinephrine concentrations (p<0.05). PBF was lower with 2% lidocaine with 1:50,000 epinephrine than with 2% lidocaine with 1:100,000 epinephrine. However, there was no significant difference in PBF and GBF reduction between the two concentrations of epinephrine (p>0.05).
When the blood flow was reduced after the injection of the anesthetics, the amplitude of the pulsatile trace recorded by laser Doppler flowmetry was smaller than that of baseline values of pulp and gingival in every tooth. Both the PBF and GBF showed rapid decreases and gradual returns toward the baseline value.
Anesthesia, as assessed by EPT, was achieved in all subjects following infiltration anesthesia using 2% lidocaine with either 1:50,000 epinephrine or 1:100,000 epinephrine. After administration of 2% lidocaine with 1:50,000 or 1:100,000 epinephrine, the threshold to EPT was increased in 1 to 5 min. Pulpal anesthesia was obtained 8.50±1.67 min after the administration of 2% lidocaine with 1:100,000 epinephrine, and 9.10±1.57 min after the injection of 2% lidocaine with 1:50,000 epinephrine. There was no significant difference in the onset of pulpal anesthesia between the two concentrations of epinephrine (p>0.05). In 70 min of observation period, 6 subjects out of 10 recovered their response to EPT in 1:100,000 epinephrine group, while 2 subjects out of 10 recovered their response in 1:50,000 epinephrine group. More subjects appeared to be recovered their response in 1:100,000 epinephrine group than in 1:50,000 epinephrine group without significance (p>0.05)
Time to minimum level of PBF and GBF and to complete loss of sensitivity to EPT after the injection of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine are presented in Fig. 6. In 1:100,000 epinephrine injection group, the time to the minimum PBF was 4.02±0.56 min, time to the minimum GBF was 10.33±2.10 min, while the time to the complete loss of sensitivity to EPT was 8.50±1.67 min. The minimum PBF was appeared first, followed by the complete loss of sensitivity to EPT, then the minimum GBF (p<0.05). In 1:50,000 epinephrine injection group, the time to the minimum PBF was 4.60± 0.92 min, time to the minimum GBF was 8.44±1.97 min, while the time to the complete loss of sensitivity to EPT was 9.10±1.57 min. There was no significant difference in the onset time (p>0.05). There was no time difference between two epinephrine concentrations both in PBF and GBF either (p>0.05). It was possible to see the recovery of PBF and GBF before the return of nervous sensation.
In three subjects with 1:50,000 epinephrine and two subjects with 1:100,000 epinephrine, decreased PBF after injection was recovered and increased above the baseline level at about 40 to 60 min after injection. An example of blood flow changes showing this phenomenon is presented in Fig 7.
IV. DISCUSSION
Blood circulation transports nutrient as well as waste product. Various research methods such as hydrogen polarography, radioactive microsphere method, intravital microscopy, 133Xenon washout method, photo plethymographic approach, thermocouple approach, and isotope fraction method have been used to examine PBF, but they are invasive and have only been used in experimental animals11-15). The development of laser Doppler flowmeter (LDF) has provided a non-invasive method of continuous monitoring changes in dental PBF. LDF was first developed to assess blood flow in tissue systems such as the skin, retina and renal cortex16). The technique utilizes a beam of infrared light produced by a laser that is directed into the tissue. As light enters the tissue, it is scattered and absorbed by moving red blood cells, and stationary tissue elements. Photons that interact with moving red blood cells are scattered and frequency shifted according to the Doppler principal. Photons that interact with stationary elements are scattered, but not Doppler shifted. A portion of the light is returned to a photo detector, and an electrical signal is produced. The electrical signal is then converted into a numerical value known as perfusion units (PU), which is proportional to blood flow, volume, and velocity. (The PU is related only to the Perimed unit). It is calibrated by means of a Motility Standard17).
The main disadvantage of laser Doppler flowmeter is that it produces a relative, rather than an absolute value of blood flow, so are not directly interpretable, the percentage of baseline must be used. Because raw values of blood flow depend on the angle of measurement and the shape and size of the tooth in laser Doppler technique, every calculation and comparison were done using the percentage value of baseline in the present study.
To have precise data from the LDF, it is important to have a consistent and reproducible placement of probe. A splint of rigid type design was essential because movement of the splint and the supported probes can induce recording artifacts. Gazelius et al.18) used modified rubber dam clamps to fix the probe, Olgart et al.19) fabricated an elastic silicone impression putty as splint, and Ban et al.20) recommended a splint made with indirect method. In the present study, the stabilizing splint to hold probe was made indirect method using silicone putty, and 3 holes were drilled. The precise fit of the probes into the drilled channels guaranteed their stability during the recording sessions. This stability was of importance as the optical fibers are not centered at the probe end; any axial rotation of the probe can produce errors during the recording sessions. Because the beams probably sense only part of the pulp, the positioning of the probes must be accurately controlled21).
Although the stabilizing splint was used, other variables, such as patient movement during deep breathing and swallowing, are difficult to eliminate. These artifacts, large spikes in reading were filtered. There were several possible causes on the large variances in subject-to-subject readings. The first cause should be the differences in pulpal and gingival circulation; another is the thickness of enamel and dentin, mineralization, and discoloration of teeth. But compared with baseline values, this could be overcome.
Buccal infiltration of 2% plain lidocaine solution caused small amount of increase in pulpal and GBF, rather than decrease, this is in agreement with the findings of Pitt Ford and McDonald22). Small amount of increase could be explained by two possible reasons. The first is by anxiety of the subject, and subsequent sympathetic activity raising cardiac output; the other is the vasodilator effect of plain lidocaine. However, it can be concluded that the reduction in laser Doppler flowmeter signals after injection of lidocaine with epinephrine, observed in every subjects was due to its vasoconstrictive action.
In comparison with baseline values, after injection of 2% lidocaine with 1:50,000 and 1:100,000 epinephrine, marked and significant reduction of blood flow in pulp and gingiva was observed. This has been explained by the fact that the epinephrine acts on the adrenergic receptors in the smooth muscle wall of the arterioles, most likely in the alveolar bone close to the site of injection, to reduce blood flow to the tissues, which the arterioles supplied5). The reduced blood flow delays the clearance of the epinephrine which may prolongs its effect. The decrease in blood flow, not only was the mean value reduced but so was the amplitude of the wave form.
Higher concentration of epinephrine appeared to induce longer period of anesthesia. Even though the time taken to minimum blood flow level was not statistically different, more subjects recovered their response to EPT in lower concentration of epinephrine group after anesthesia. This implies that even though the penetration potential of epinephrine to pulpal vessel may not be different between two concentrations of epinephrine, higher concentration of epinephrine may prolong anesthetic effect.
In gingiva, the difference of epinephrine concentration did not show any significant difference in the reduction of blood flow. The time to the minimum level of GBF was not different between two concentrations of epinephrine either. Presumably, higher concentration of epinephrine may have induced more reduction of GBF. However, more magnitude of collateral circulation of gingiva may have masked its difference.
Ketabi et al.23) produced a dose response curve for lidocaine with 1:80,000 epinephrine to establish the standard volume to be injected. They chose 0.5 ml of lidocaine with epinephrine as the standard dose to be injected because it caused more than 30% reduction in laser Doppler flowmeter signals at gingiva. In the present study, since pulp as well as gingiva was planned to record, somewhat more solution of anesthetics, that was 0.9 ml, was used in each subject, which is the amount, which is usually administered to obtain anesthesia for dental procedures. This more amount of anesthetics may be another possible reason of no difference between two epinephrine concentrations in GBF.
PBF rate was the highest of all oral tissues in an animal study using radioisotope-labeled microspheres7). In contrast, the data from the present study on humans showed that the baseline GBF was greater than the baseline PBF. This contradiction is likely due to the enamel and dentin of the tooth, which decreases the detection of the blood flow by the laser Doppler flowmeter. The blood vessels of the gingiva are in closer proximity to the surface tissue and to the laser Doppler probe, which would then give a higher perfusion unit reading.
In three subjects with 1:50,000 epinephrine and two subjects with 1:100,000 epinephrine, decreased PBF after injection was recovered and increased above the baseline level at about 40 to 60 min after injection. This phenomenon may be explained by Pitt Ford and McDonald22) who considered it as a pulpal hyperemia following the return of blood flow. Hyperemia is a normal response following vasoconstriction, but does not appear to have been demonstrated previously following dental local anesthesia in man. This is an area for further investigation.
The maximum reduction in blood flow was approximately half of that reported by Kim et al.24) in an animal study. There is possible explanation. Kim et al.24) used 15 m microspheres as tracers, and these were twice the diameter of erythrocytes, therefore vasoconstriction may have had a more marked effect on these spheres.
The exact manner by which local anesthetic drug interrupts nerve conduction is much more clearly understood than before and the action of local anesthetics may be explained, at least potentially within the framework of the ionic theory of nervous activity proposed by Hodgkin et al. in 195225). As a result of better understanding of nerve conduction, several theories have been postulated to explain the exact mechanism of local anesthetics, such as membrane expansion theory, specific receptor theory, neutralization of transmembrane charge theory, and calcium competition theory26).
A number of separate studies on microcirculation and sensory nerve activity in the dental pulp have shown their interrelationship, and several investigators stated that local microcirculatory changes may have profound effects on sensory nerve functions in the pulp7, 27-30). A severe reduction in PBF by the apical injection of epinephrine resulted in concomitant decreases in intradental sensory nerve activity27,31). The fast-conducting A fibers lose their function rapidly as a result of ischemia, to which the slowconducting C fibers are less sensitive32). This suggests that C fibers may maintain their functional capacity longer than A-delta fibers during inflammation, in which PBF and therefore oxygen content are reduced as a result of the low compliance system of the pulp29,33). Therefore, it is probable that loss of sensitivity to EPT was influenced by two factors. One is anesthetic effect of 2% lidocaine itself, and the other is reduced PBF, which causes inhibitory action on excitability of A-delta fibers.
Dental procedures such as cavity preparations are usually performed after administration of local anesthetics with vasoconstrictors and may cause inflammatory changes in the dental pulp. Clearance of pulpal toxins is related to the pulpal circulation, and the reduction of PBF can result in excessive accumulation of heat and inflammatory mediators, such as prostaglandins and serotonin7). This accumulation may lead to local inflammation and possible pulpal necrosis. Inadequate oxygen supply to the pulpal tissue with vasoconstriction is possible. This also may lead to direct pulpal necrosis. Kim34) reported that the ligamental injection using 2% lidocaine with 1:100,000 epinephrine caused a complete cessation of flow in the microcirculation of the rat incisor tooth. The injection with the same anesthetic also caused a complete stop in the PBF in dogs for more than 20 min. In the present study, infiltration anesthesia caused 47 to 57% reduction of PBF in both concentrations of epinephrine. Although the evidence that the ligamental injection causes pulpal death is not conclusive, it would like to recommend clinicians not to use the ligamental injection for restorative procedures on teeth with vital pulps. These considerations indicate that attempts should be made to maintain an optimum PBF during dental restorative procedures.
There were several difficulties encountered during the study in human. Because the duration of the procedure was lengthy, it was hard for the volunteers to keep the splint over 1 hour without any movement. They needed patience to control their movements of their heads and bodies that may be related to sympathetic nerve activation. Difficulties were also encountered when administering the local anesthetic. Because the splint could not removed during procedures to prevent changes in probe angle and position, it was difficult to inject local anesthetic at the same point in each subject.
In conclusion, 2% lidocaine with both 1:50,000 and 1:100,000 epinephrine significantly reduced PBF and GBF. Higher concentration of epinephrine reduced more PBF than with lower concentration of epinephrine, and GBF was reduced more significantly than PBF with the same concentration of epinephrine. Further investigation is needed to understand how the higher concentration of epinephrine can control the surgical hemorrhage more effectively even though the GBF appeared not significantly different.
V. CONCLUSION
Local anesthetics are used not only in conventional endodontic treatment to control pain during pulp extirpation but also in surgical endodontic treatment to control hemorrhage. For the control of hemorrhage, relatively higher concentration of epinephrine is used in surgical endodontics in conjunction with local anesthetics while lower concentration of epinephrine is used in nonsurgical endodontics. For the use of epinephrine in local anesthetics, we need to understand the effect of its concentration on the pulpal (PBF) and gingival blood flow (GBF), and their relation to pulpal numbness. The purpose of the study was to evaluate the influence of epinephrine concentration on the PBF and GBF, and their relation to pulpal numbness induced by local anesthesia by simultaneous recording of both blood flows and pulpal response to electrical stimulus.
Maxillary left central incisors of ten volunteers aged 24 to 27 were used. For the stabilization of laser Doppler flowmeter probes, stabilizing splints were fabricated using vinyl polysiloxane impression putty to minimize movement artifacts and to allow correct repositioning of the probe. For the measurement of PBF and GBF, a laser Doppler flowmeter (Periflux 4001, Perimed Co., Stockholm, Sweden) was used with a dental probe toward the labial surface of the crown and a standard probe toward the labial attached gingiva. 2% plain lidocaine without epinephrine was used as a control, and 2% lidocaine with 1:50,000 epinephrine and 1:100,000 were used on each subject. Buccal infiltrations were given with a 27-gauge needle placed in the submucosa over the estimated position of the root apex. After giving the local anesthetics, PBF and GBF were recorded simultaneously and continuously for 70 min. Threshold values to the electric pulp testing (EPT) were recorded manually. Pulpal numbness was considered achieved when the subject gave no response to the maximum output (64 machine units) of the pulp tester. The paired variables of control and experimental data were analyzed using paired t-test, Wilcoxon's signed rank test, Duncan's multiple range test, and Fisher's exact test.
When 2% plain lidocaine was injected without epinephrine as a control, PBF and GBF showed little change. Administration of 2% lidocaine with both concentrations of epinephrine induced significant reduction of PBF and GBF (p<0.05) along with decreased amplitude of the pulsatile trace recorded by laser Doppler flowmeter. PBF was appeared to be decreased more with 2% lidocaine with 1:50,000 epinephrine than with 2% lidocaine with 1:100,000 epinephrine. However, there was no significant difference in PBF and GBF reduction between the two concentrations of epinephrine (p>0.05). GBF was significantly more decreased than the PBF in both epinephrine concentrations (p<0.05). There was no significant difference in the onset of pulpal anesthesia tested by EPT between the two concentrations of epinephrine (p>0.05). Time to minimum level of PBF was earlier than that of GBF (p<0.05) in both concentrations of epinephrine. However, there was no time difference between two epinephrine concentrations both in PBF and GBF (p>0.05). The minimum PBF was appeared first followed by the complete loss of sensitivity to EPT, then the minimum GBF in 1:100,000 epinephrine group (p<0.05). In the limited time of observation period, 1:50,000 epinephrine induced longer anesthetic effect than 1:100,000 epinephrine without significance (p>0.05).
- 1. Cawson RA, Curson I, Whittington DR. The hazards of dental local anesthetics. Br Dent J. 1983;154: 253-258.ArticlePubMedPDF
- 2. Gray RJM, Lomax AM, Rood JP. Periodontal ligament injection: with or without a vasoconstrictor? Br Dent J. 1987;162: 263-265.ArticlePubMedPDF
- 3. Sisk AL. Vasoconstrictors in local anesthesia for dentistry. Anesth Prog. 1993;39: 187-193.
- 4. Kim S, Rethnam S. Hemostasis in endodontic microsurgery. Dent Clin Nor Am. 1997;41: 499-511.Article
- 5. Kim S. In: Kim S, editor. Anesthesia and hemostasis. Color Atlas of Microsurgery in Endodontics. 2001;Philadelphia: Saunders; 63-71.
- 6. Kim S. In: Stephen C, Richard CB, editors. Endodontic microsurgery. Pathways of the pulp. 2002;8th ed. St. Louis: Mosby; 693-696.
- 7. Kim S. Regulation of pulpal blood flow. J Dent Res. 1985;64(Special Issue):590-596.ArticlePubMedPDF
- 8. Ebihara A, Suda H. PBF assessed by laser Doppler flowmetry in a tooth with a horizontal root fracture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81: 229-233.PubMed
- 9. Gazelius B, Edwall L. Restored vitality in luxated teeth assessed by laser Doppler flowmeter. Endod Dent Traumatol. 1988;4: 265-268.ArticlePubMed
- 10. Watson ADM, Pitt Ford TR, McDonald F. Blood flow changes in the dental pulp during limited exercise measured by laser Doppler flowmetry. Int Endod J. 1992;25: 82-87.ArticlePubMed
- 11. Meyer MW, Path MG. Blood flow in the dental pulp of dogs determined by hydrogen polarography and radioactive microsphere methods. Arch Oral Biol. 1979;24: 601-605.ArticlePubMed
- 12. Pohto M, Scheinin A. Microscopic observation on living dental pulp, 1. Method for intravital study of circulation in rat incisor pulp. Acta Odontol Scand. 1958;16: 303-314.
- 13. Kim S, Lipowsky HH, Usami S, Chien S. Arteriovenous distribution of hemodynamic parameters in the rat dental pulp. Microvasc Res. 1984;27: 28-38.ArticlePubMed
- 14. Kim S, Liu M, Markowitz K, Bilotto G, Kim JD. Comparison of pulpal blood flow in dog canine teeth determined by the laser Doppler and 133Xenon washout methods. Arch Oral Biol. 1990;35: 411-413.PubMed
- 15. Meyer MW. Methodologies for studying pulpal hemodynamics. J Endod. 1980;6: 466-472.ArticlePubMed
- 16. Riva C, Ross B, Benedek GB. Laser Doppler measurements of blood flow in capillary tubes and retinal arteries. Invest Ophthalmol. 1972;11: 936-944.PubMed
- 17. Perimed . The art of microvascular perfusion measurements. User's manual. 1993.
- 18. Gazelius B, Olgart L, Edwall B. Noninvasive recording of blood flow in human dental pulp. Endod Dent Traumatol. 1986;2: 219-221.ArticlePubMed
- 19. Olgart L, Gazelius B, Lindh-Stromberg U. Laser Doppler flowmetry in assessing vitality in luxated permanent teeth. Int Endod J. 1988;21: 300-306.ArticlePubMed
- 20. Ban TW, Kim SK. Measurement of pulpal blood flow using a laser Doppler flowmeter. J Korean Acad Conserv Dent. 1999;24: 560-569.
- 21. Ingolfsson A, Tronstad L, Hersh E, Riva C. Effect of probe design on the suitability of laser Doppler flowmetry in vitality testing of human teeth. Endod Dent Traumatol. 1993;9: 65-70.ArticlePubMed
- 22. Pitt Ford TR, McDonald F. Action of adrenaline on the effect of dental local anesthetic solutions. Endod Dent Traumatol. 1993;9: 31-35.PubMed
- 23. Ketabi M, Hirsch RS. The effects of local anesthetic containing adrenaline on gingival blood flow in smokers and non-smokers. J Clin Periodontol. 1997;24: 888-892.ArticlePubMed
- 24. Kim S, Edwall L, Trowbridge H, Chien S. Effects of local anesthetics on pulpal blood flow in dogs. J Dent Res. 1984;63: 650-652.ArticlePubMedPDF
- 25. Hodgkin A, Huxley F. A quantitative description of membrane current and its application to conduction and excitation in nerve. J Physiol. 1952;117: 500-544.ArticlePubMedPMCPDF
- 26. Bennett CR. Monheim's local anesthesia and pain control in dental practice. 1978;6th ed. St. Louis: Mosby; 64-67.
- 27. Edwall L, Scott D Jr. Influence of changes in microcirculation on the excitability of the sensory unit in the tooth of the cat. Acta Physiol Scand. 1971;82: 55-56.Article
- 28. Olgart L. Excitation of intradental sensory units by pharmacological agents. Acta Physiol Scand. 1974;92: 48-55.ArticlePubMed
- 29. Olgart L. The role of local factors in dentin and pulp in intradental pain mechanisms. J Dent Res. 1985;64(Special Issue):572-578.ArticlePubMedPDF
- 30. Gazelius B. Studies on the release and effects of putative mediators of pain in the dental pulp. 1981;Stockholm, Sweden: Karolinska Institute; [Thesis].
- 31. Olgart L, Gazelius B. Effects of adrenaline and felypressin (Octapressin) on blood flow and sensory nerve activity in the tooth. Acta Odontol Scand. 1977;35: 69-75.ArticlePubMed
- 32. Tonder K, Kvinnsland I. Micropuncture measurements of interstitial fluid pressure in normal and inflamed dental pulp in cats. J Endodont. 1983;9: 105-109.Article
- 33. Jyvasjarvi E, Narhi M, Virtanen A. Differential blockade of intradental A-delta fibers by ischemia. J Dent Res. 1983;62(Special Issue):35.
- 34. Kim S. Ligamental injection: A physiological explanation of its efficacy. J Endod. 1986;12: 486-491.PubMed
REFERENCES
Fig. 1

Flow chart recording of the changes in pulpal blood flow and gingival blood flow following injection of 2% lidocaine with 1:100,000 epinephrine. The arrows show the time of the injection (Inj).

Fig. 2

Flow chart recording of the changes in pulpal blood flow and gingival blood flow following injection of 2% lidocaine with 1:50,000 epinephrine. The arrows show the time of the injection (Inj).

Fig. 3

Graph of the changes in pulpal blood flow (PBF), gingival blood flow (GBF), and electric pulp testing (EPT) values following an injection of 2% lidocaine with 1:100,000 epinephrine.

Fig. 4

Graph of the changes in pulpal blood flow (PBF), gingival blood flow (GBF), and electric pulp testing (EPT) values following an injection of 2% lidocaine with 1:50,000 epinephrine.

Fig. 5

Effects of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine on pulpal and gingival blood flows. Data are shown as percentage blood flows from the baseline values, and Mean +/- SEM. n=10. Infiltrative injection (0.9 ml) in the buccal mucosa significantly reduced both pulpal and gingival blood flows (p<0.05). Reduction of pulpal blood flow was in a dose-dependent pattern (p<0.05).

Fig. 6

Effects of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine on the induction time to the minimum level of pulpal (PBF) and gingival blood flows (GBF), and time to complete loss of sensitivity to electric pulp test (EPT) after injection. Data are shown as time in min after injection, and Mean +/- SEM. n=10. After buccal injection of 2% lidocaine with 1:100,000 epinephrine, complete loss of sensitivity to EPT was preceded by the maximum reduction of PBF and followed by the maximum reduction of GBF.

Tables & Figures
REFERENCES
Citations
Citations to this article as recorded by 

- Biologic response of local hemostatic agents used in endodontic microsurgery
Youngjune Jang, Hyeon Kim, Byoung-Duck Roh, Euiseong Kim
Restorative Dentistry & Endodontics.2014; 39(2): 79. CrossRef - Cardiovascular effect of epinephrine in endodontic microsurgery: a review
Youngjune Jang, Euiseong Kim
Restorative Dentistry & Endodontics.2013; 38(4): 187. CrossRef - Effect of local anesthesia on pulpal blood flow in mechanically stimulated teeth
Wan-Sik Chu, Seung-Ho Park, Dong-Kuk Ahn, Sung Kyo Kim
Journal of Korean Academy of Conservative Dentistry.2006; 31(4): 257. CrossRef
The influence of epinephrine concentration in local anesthetics on pulpal and gingival blood flows





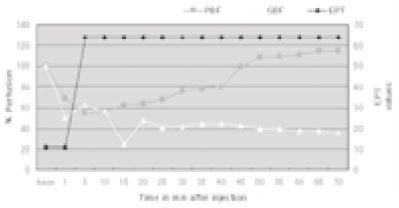
Fig. 1
Flow chart recording of the changes in pulpal blood flow and gingival blood flow following injection of 2% lidocaine with 1:100,000 epinephrine. The arrows show the time of the injection (Inj).
Fig. 2
Flow chart recording of the changes in pulpal blood flow and gingival blood flow following injection of 2% lidocaine with 1:50,000 epinephrine. The arrows show the time of the injection (Inj).
Fig. 3
Graph of the changes in pulpal blood flow (PBF), gingival blood flow (GBF), and electric pulp testing (EPT) values following an injection of 2% lidocaine with 1:100,000 epinephrine.
Fig. 4
Graph of the changes in pulpal blood flow (PBF), gingival blood flow (GBF), and electric pulp testing (EPT) values following an injection of 2% lidocaine with 1:50,000 epinephrine.
Fig. 5
Effects of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine on pulpal and gingival blood flows. Data are shown as percentage blood flows from the baseline values, and Mean +/- SEM. n=10. Infiltrative injection (0.9 ml) in the buccal mucosa significantly reduced both pulpal and gingival blood flows (p<0.05). Reduction of pulpal blood flow was in a dose-dependent pattern (p<0.05).
Fig. 6
Effects of 2% lidocaine with 1:100,000 and 1:50,000 epinephrine on the induction time to the minimum level of pulpal (PBF) and gingival blood flows (GBF), and time to complete loss of sensitivity to electric pulp test (EPT) after injection. Data are shown as time in min after injection, and Mean +/- SEM. n=10. After buccal injection of 2% lidocaine with 1:100,000 epinephrine, complete loss of sensitivity to EPT was preceded by the maximum reduction of PBF and followed by the maximum reduction of GBF.
Fig. 7
An example of changes in pulpal blood flow (PBF), gingival blood flow (GBF), and electric pulp testing (EPT) values following injection of 2% lidocaine with 1:50,000 epinephrine. Note the decreased PBF was recovered and increased above the baseline level at about 45 min after injection.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
The influence of epinephrine concentration in local anesthetics on pulpal and gingival blood flows

 KACD
KACD
 ePub Link
ePub Link Cite
Cite