Abstract
-
Objectives
This in vitro study aimed to evaluate temperature variation on the external surface of mandibular molars and within ultrasonic inserts when using adapter-coupled versus one-piece inserts.
-
Methods
Twenty-four extracted human mandibular molars were divided into two groups based on the type of ultrasonic insert used: adapter-coupled and one-piece inserts. Temperature on the external surface of each tooth was measured with a thermocouple probe positioned in the furcation area, capturing data continuously. The temperature of the ultrasonic inserts was monitored in real-time using a thermal imaging camera. Measurements were taken in a controlled environment without cooling for over 120 seconds. Statistical analysis was conducted using analysis of variance (ANOVA) and two-way ANOVA with repeated measures to evaluate temperature variations between groups and over time, with significance set at 5%.
-
Results
In the external tooth surface temperature measurements, no significant differences were observed between the groups during the initial 15 seconds (p = 0.185) and 30 seconds (p = 0.067). However, significant differences emerged at 60 seconds (p = 0.025), 90 seconds (p = 0.024), and 120 seconds (p = 0.020), with the one-piece insert group demonstrating higher temperatures in the furcation region. Thermal imaging of the inserts revealed a significant difference at all time points (p < 0.001), with adapter-coupled inserts showing greater heating.
-
Conclusions
The use of ultrasonic inserts leads to a gradual rise in temperature on the external tooth surface. One-piece inserts generated higher temperatures on the tooth, while adapter-coupled inserts exhibited greater heating within the insert.
-
Keywords: Endodontics; Dental instruments; Molar; Temperature; Thermal conductivity; Ultrasonics
INTRODUCTION
Ultrasonic technology offers a wide range of applications in endodontics, making it an invaluable tool for enhancing root canal treatment [
1], retreatment [
2,
3], and endodontic surgery [
4,
5]. Its uses include refining access to root canals [
6,
7], locating hidden canals [
8,
9], and effectively removing pulp calcifications and nodules that may otherwise hinder treatment [
10,
11]. Furthermore, ultrasonics assists in the removal of fractured instruments [
12,
13] and root canal posts [
14,
15] and can prepare areas that traditional instruments struggle to reach, such as isthmuses and flattened canal spaces, thus improving overall cleaning efficacy [
16,
17]. Ultrasonics is also frequently employed to activate irrigating solutions, increasing their penetration and effectiveness [
18,
19], and is used in obturation procedures for cutting and condensing gutta-percha [
20,
21].
Ultrasonics operates by converting electrical energy into high-frequency mechanical vibrations through an ultrasonic insert, a process that can generate heat as vibrational energy dissipates within surrounding tissues and fluids [
22]. This heat buildup, if excessive or prolonged, may pose a risk to periodontal structures. When the ultrasonic insert contacts dentin, additional frictional forces can generate even more heat within the tooth structure [
23–
27]. Excessive heating, if sufficiently intense and/or prolonged, may damage the periodontal ligament and alveolar bone [
28,
29].
In many of these procedures, continuous cooling is often avoided to maintain clear visualization of the operative field and ensure procedural accuracy. However, without cooling, significant temperature increases can occur in both the tooth structure and surrounding tissues, potentially reaching levels that pose risks to periodontal health [
29]. The degree of heat generation varies based on several factors, including the type of ultrasonic insert, power settings, and duration of activation [
25]. Despite these known risks, there is a notable lack of studies that quantify the extent of temperature rise in procedures without continuous cooling. A clearer understanding of these thermal effects is essential to establish safer protocols and refine guidelines for procedures where cooling is limited, ultimately protecting patient outcomes and periodontal integrity.
Therefore, the aim of this in vitro study was to evaluate temperature variation on the external surface of mandibular molars when using adapter-coupled inserts and one-piece inserts, both operated without cooling for 120 seconds. Additionally, temperature variation within the ultrasonic insert itself during use was assessed. The null hypothesis tested posited that no significant difference in temperature variation would be observed between the different types of inserts.
METHODS
Sample calculation
Sample size calculation was conducted using the program G*Power v3.1 for Mac (Heinrich Heine, University of Düsseldorf), based on analysis of variance (ANOVA) with repeated measures. An effect size of 1.78, an alpha error of 0.05, and a power of 95% were set for the calculation. Results indicated that 12 samples per group would be sufficient to detect significant differences.
Sample selection and specimen preparation
This study was approved by the Institutional Research Ethics Committee of Universidade Positivo (CAAE 76141723.6.0000.0093).
Twenty-four extracted human mandibular molars with two roots were selected. The teeth were cleaned, and the crown was opened with round burs until the pulp chamber floor was fully exposed. Radiographs were taken with a digital sensor (Snapshot; Instrumentarium Dental, Tuusula, Finland) using an exposure time of 0.3 seconds and a focal length of 30 cm. The thickness of the furcation wall was measured in millimeters on the radiographs, with all measurements performed by a single operator.
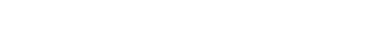
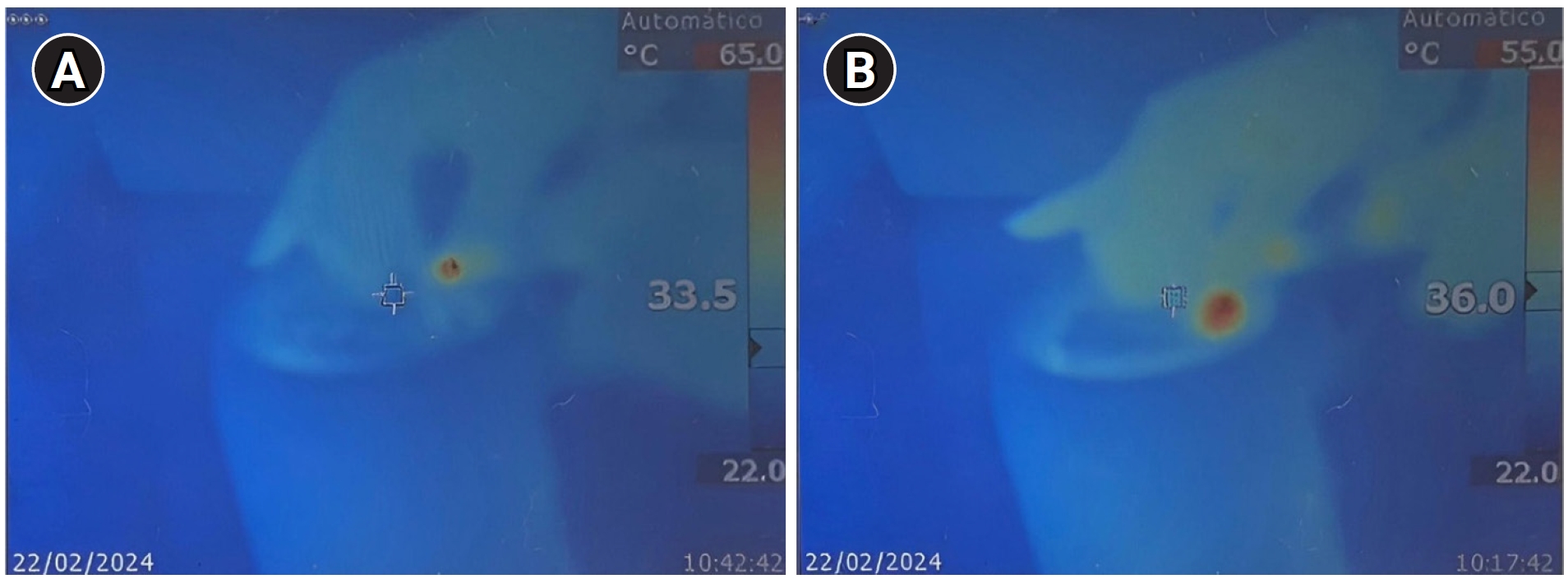
The teeth were paired to create 12 pairs with similar furcation thicknesses. One tooth from each pair was randomly assigned to either the adapter-coupled or one-piece insert group (
Figure 1).
- Adapter-coupled group: adapter + spherical diamond insert (Dental Trinks, São Paulo, Brazil) (n = 12)
- One-piece insert group: spherical diamond insert (Dental Trinks) (n = 12)
A total of 24 inserts from the same manufacturer were used, 12 from each model, with a single insert designated for each tooth. The teeth were stored in distilled water at 37°C until the time of the experiment.
Use of ultrasonic inserts
The experiment was conducted in a room with controlled temperature and humidity. Each specimen was fixed in floral foam, immersed in water, and maintained at 35°C in a bottle warmer. A thermocouple tip (type K universal MTK-01; Minipa do Brasil, São Paulo, Brazil) connected to an Arduino UNO R3 data acquisition device (Arduino, Ivrea, Italy) was positioned between the floral foam and the furcation area of the tooth. This setup transmitted the temperature-time profile to a computer, enabling continuous recording of temperature changes on the root’s outer surface every second for 120 seconds.
A thermal imaging camera (Ti9; Fluke, Everett, WA, USA) was used to record the temperature variation in the ultrasonic insert during use. The camera was mounted on a support at a distance of 50 cm from the experimental setup.
Ultrasonic activation was performed using an ultrasonic unit (P5 XS Bled Newtron; Satelec Acteon, Mérignac, France) set at a power level of 10, corresponding to 50% of the device’s maximum power output. Each insert was moved in a linear motion within the furcation region of the tooth, with a 3-mm forward and backward amplitude, maintained throughout the experiment. To standardize the ultrasonic action, the transducer was attached to a device that enabled precise 3 mm horizontal movement on each tooth.
This procedure was performed by a single trained operator with 20 years of experience in endodontics. The temperature variation of the tooth surface and ultrasonic insert was evaluated at 15, 30, 60, 90, and 120-second intervals for the two groups.
Statistical analysis
Data were analyzed using Jamovi software, ver. 1.6 (The Jamovi Project, 2021). Normality was assessed with the Shapiro-Wilk test, confirming a normal distribution. Temperature variation was evaluated using ANOVA, followed by the Tukey test for multiple comparisons. A two-factor ANOVA with repeated measures was conducted to analyze the effect of time within each group. The significance level was set at 5%.
RESULTS
On the external tooth surface, no statistically significant difference between the groups was observed at 15 seconds (
p = 0.185) and 30 seconds (
p = 0.067). However, significant differences emerged at 60 seconds (
p = 0.025), 90 seconds (
p = 0.024), and 120 seconds (
p = 0.020), with one-piece inserts recording higher temperatures across all intervals. At 120 seconds, the average temperature for one-piece inserts reached 55.6°C ± 9.06°C, while adapter-coupled inserts averaged 48.3°C ± 4.50°C (
Table 1).
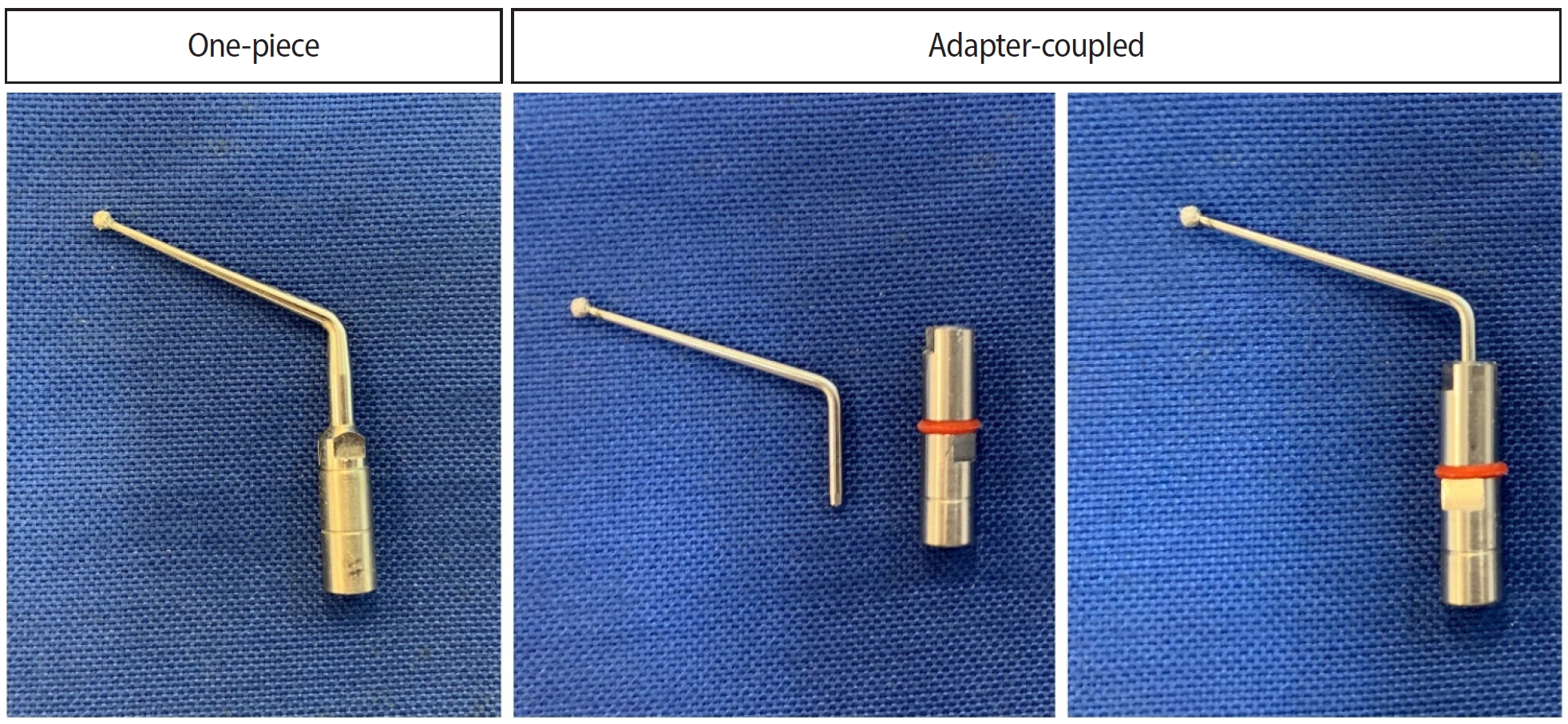
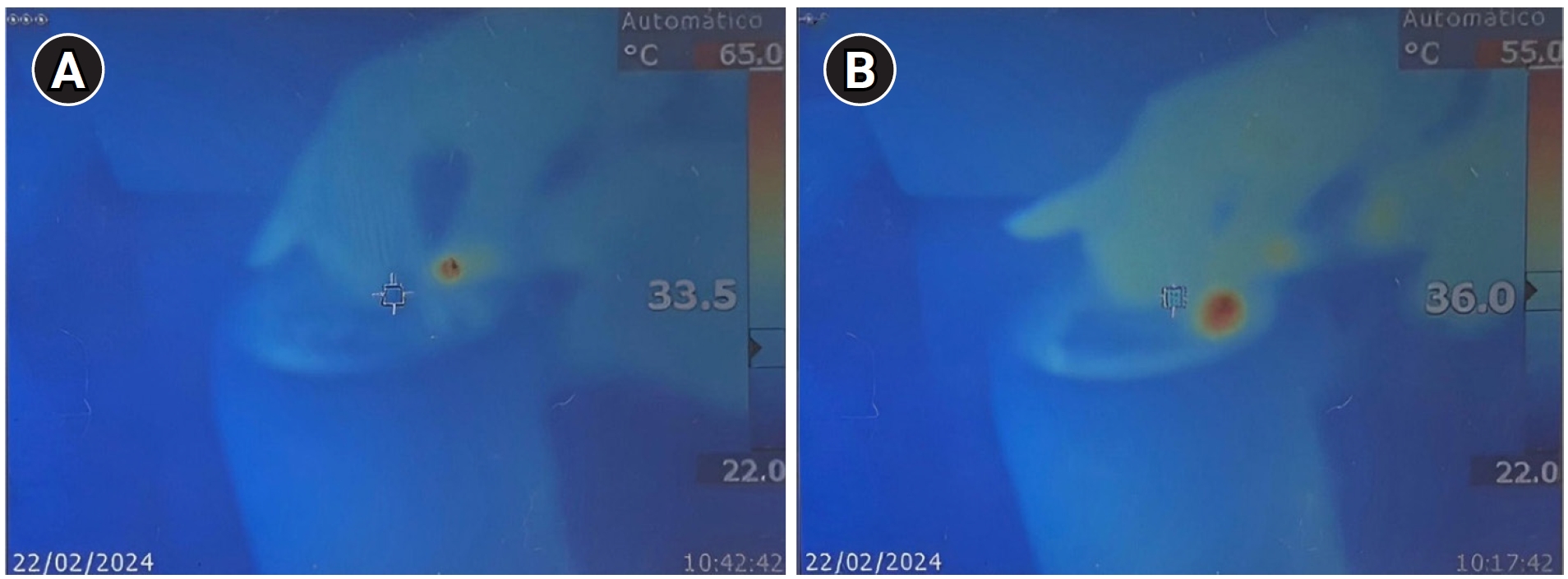
Regarding the temperature of the ultrasonic insert itself, statistically significant differences were observed across all evaluated intervals (p < 0.001), with adapter-coupled inserts exhibiting higher temperatures throughout. At 120 seconds, the average temperature reached 58.5 ± 7.99°C in the adapter-coupled group, compared to 46.4 ± 4.74°C in the one-piece group. Furthermore, within each group, a consistent temperature increase was observed with prolonged activation time (p < 0.001).
Thermal images captured during the experiment showed that, for adapter-coupled inserts, the highest temperatures were concentrated at the junction between the adapter and the insert. In contrast, for one-piece inserts, the greatest heating occurred at the point of contact between the insert and the tooth.
Figure 2 illustrates these differences, highlighting the areas of maximum temperature for each insert type.
DISCUSSION
The aim of this study was to assess temperature variation on the external surface of mandibular molars when using adapter-coupled inserts compared to one-piece inserts over a 120-second period. The null hypothesis was partially rejected, as significant differences in heating were found between the two insert types. Notably, after 60 seconds of continuous activation, the tooth temperature showed a significant increase in the one-piece insert group compared to the adapter-coupled group (
Table 1).
A progressive temperature increase was observed with prolonged activation time, a finding of clinical relevance as these values exceeded critical thresholds for maintaining the viability of dental tissues. Temperatures exceeding 43°C— recorded as early as 30 seconds after activation— are particularly concerning, as they have been associated with periodontal ligament necrosis [
30], dental ankylosis [
31], and bone resorption [
28] The periodontal ligament, a delicate connective tissue with limited regenerative capacity, is especially vulnerable to thermal damage. Unlike mineralized tissues, which may tolerate brief periods of elevated temperature, the periodontal ligament is more susceptible due to its rich vascular and cellular components. Sustained heating can compromise its blood supply and structural integrity, potentially leading to irreversible injury [
30,
31]. These findings underscore the risk posed to periodontal and periapical tissues during extended ultrasonic activation and highlight the critical importance of effective cooling strategies. In the absence of adequate cooling, the likelihood of thermal injury to the periodontal ligament becomes clinically relevant.These results are consistent with previous studies that also demonstrated cumulative temperature rises with ultrasonic use [
24–
27].
To mitigate the risk of thermal damage to tissues adjacent to the tooth during ultrasonic use, continuous irrigation is widely recommended [
22–
26,
32]. However, in various endodontic procedures—such as refining root canal access, locating canals, removing pulp calcifications and nodules, cutting and condensing gutta-percha, and performing endodontic retreatments—continuous irrigation is impractical, as it can obscure visualization and, in some cases, impede the procedure itself. To counteract potential thermal risks, periodic ultrasonic activation is recommended, with interruptions every 30 seconds to allow for irrigation and cooling [
10,
33].
In this study, temperatures exceeding 43°C were recorded after just 30 seconds of continuous ultrasonic use. Based on these findings, it is recommended to take breaks for irrigation and cooling every 15 seconds, as this interval provides sufficient working time while reducing the risk of reaching harmful temperature levels. The results also highlight considerable heating of the ultrasonic inserts themselves. Thermal imaging showed that in the adapter group, peak temperatures occurred at the junction between the adapter and the insert, while in the one-piece group, the highest temperatures were observed at the contact point between the insert and the tooth.
Although cutting effectiveness was not the primary focus of this study, an observed difference between inserts with adapters and one-piece inserts raises interesting considerations. While adapters offer cost benefits and enable tip interchangeability, they may dampen the vibration of the inserts, particularly at lower power settings [
34]. In this study, the reduced heating of teeth observed when using inserts with adapters suggests that some vibrational energy may dissipate at the adapter-insert junction, potentially impacting cutting efficiency. However, it is important to note that these observations are qualitative rather than quantitatively substantiated. Future studies with precise quantitative analyses are necessary to confirm this effect and evaluate its clinical significance, particularly for cases requiring high cutting precision. Furthermore, research is needed to assess how cutting effectiveness, the amount of material removed, and the remaining dentin thickness influence the heat generated and transmitted to the periodontal ligament and alveolar bone. This insight may assist endodontists in selecting the most appropriate insert, especially in cases requiring high cutting precision.
In this study, a stainless steel, spherical diamond insert was selected due to its versatility, making it suitable for a broad range of clinical applications, including canal localization, removal of coronal obstructions, restorative materials, calcifications, and both temporary and permanent cements. Nonetheless, ultrasonic inserts differ considerably in design and material composition, factors that may significantly influence their thermal behavior during clinical use. Therefore, further studies are warranted to explore the thermal profiles of inserts with varying geometries and materials, aiming to generate evidence-based recommendations for optimal insert selection according to specific clinical scenarios.
Although this study provides valuable data on the heat generated during ultrasonic use in endodontics, several limitations should be noted. First, the in vitro nature of the study cannot fully replicate the complex dynamics present in the clinical environment, where variables such as tissue type and individual anatomical differences may influence temperature dissipation. Additionally, while we observed differences in heat generation between one-piece and adapter-coupled inserts, the exact impact of these temperature variations on adjacent tissues, particularly over extended periods, remains unclear. Future studies should explore the effects of sustained ultrasonic use on periodontal ligament and alveolar bone cells to determine the clinical significance of elevated temperatures. Furthermore, it would be beneficial to investigate how temperature varies across different power settings, insert designs, and irrigation techniques. Finally, expanding this research to include a variety of ultrasonic insert designs and coupling systems could offer a more comprehensive understanding of safety and efficacy, ultimately guiding clinicians in selecting the most appropriate tools for specific endodontic procedures.
This study highlights the importance of managing heat generation during the use of ultrasonic inserts in endodontics. While efficient cutting is crucial for procedures such as root canal access refinement and calcification removal, our findings confirm that ultrasonic activation, particularly with one-piece inserts, can rapidly increase temperatures to levels that may jeopardize periodontal and surrounding tissue health. Clinically, this underscores the need for incorporating cooling pauses and, when feasible, intermittent irrigation to mitigate thermal buildup. By balancing effective cutting with thermal management strategies, clinicians can perform ultrasonic procedures with greater safety, reducing the risk of thermal injury while maintaining the efficiency needed for precise endodontic work.
CONCLUSIONS
The use of spherical ultrasonic inserts leads to a gradual rise in temperature on the external tooth surface. One-piece inserts generated higher temperatures on the tooth, while adapter-coupled inserts exhibited greater heating within a spherical insert.
-
CONFLICT OF INTEREST
Emmanuel João Nogueira Leal da Silva is the Associate Editor of Restorative Dentistry and Endodontics and was not involved in the review process of this article. The authors declare no other conflicts of interest.
-
FUNDING/SUPPORT
The authors have no financial relationships relevant to this article to disclose.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Crozeta BM, Marques-da-Silva B, Tomazinho FSF, Diógenes AN. Investigation: Crozeta BM, Marques-da-Silva B. Methodology: Brotto GL, Tomazinho FSF. Supervision: Tomazinho FSF, Diógenes AN. Validation: Diógenes AN. Writing - original draft: Brotto GL, Tomazinho FSF. Writing - review & editing: Crozeta BM, Silva EJNL. All authors read and approved the final manuscript.
-
DATA SHARING STATEMENT
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
Figure 1.Ultrasonic inserts used in the study. Spherical diamond insert in one-piece insert and adapter + spherical diamond insert in adapter-coupled inserts.
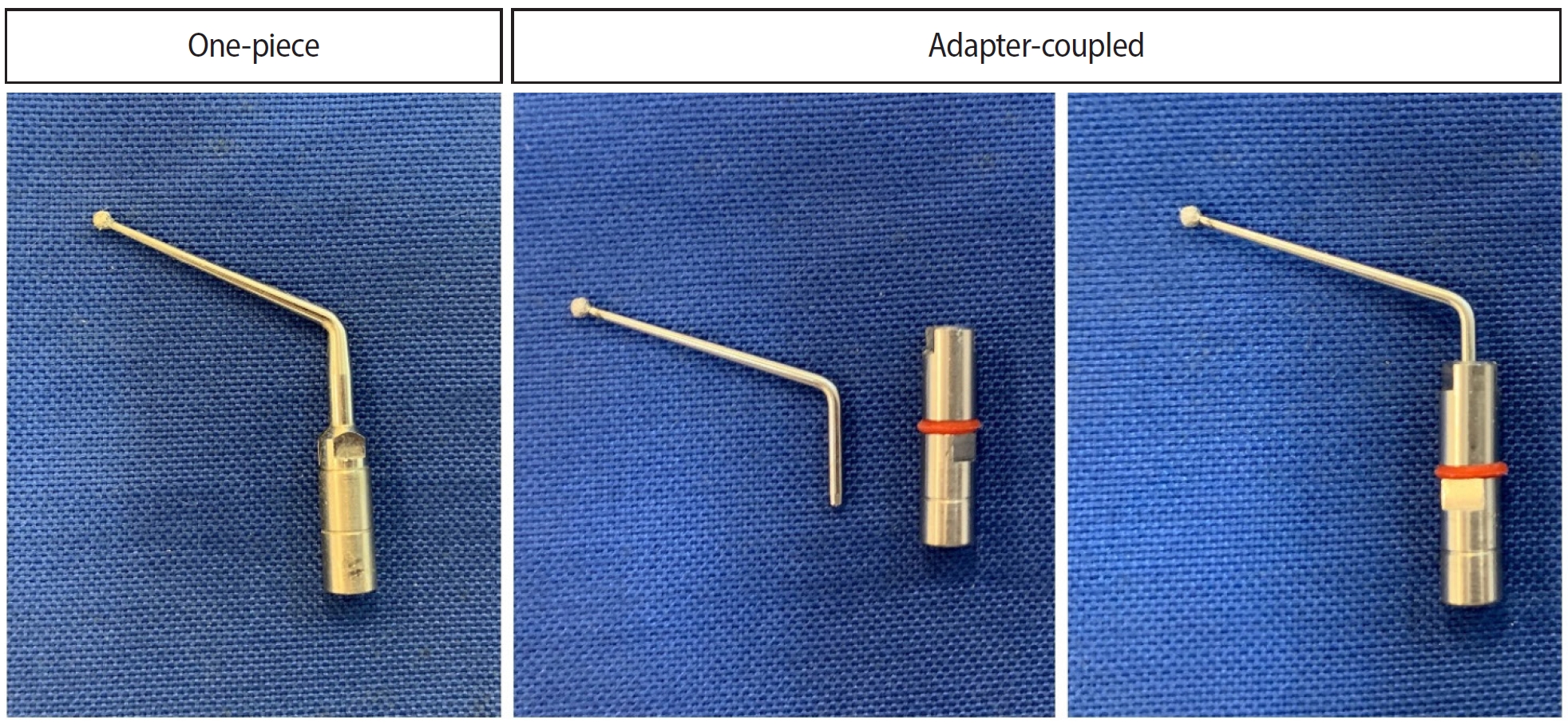
Figure 2.Thermal images captured during the experiment. (A) Adapter-coupled inserts. The highest temperatures were concentrated at the junction between the adapter and the insert. (B) One-piece inserts. The greatest heating occurred at the point of contact between the insert and the tooth.
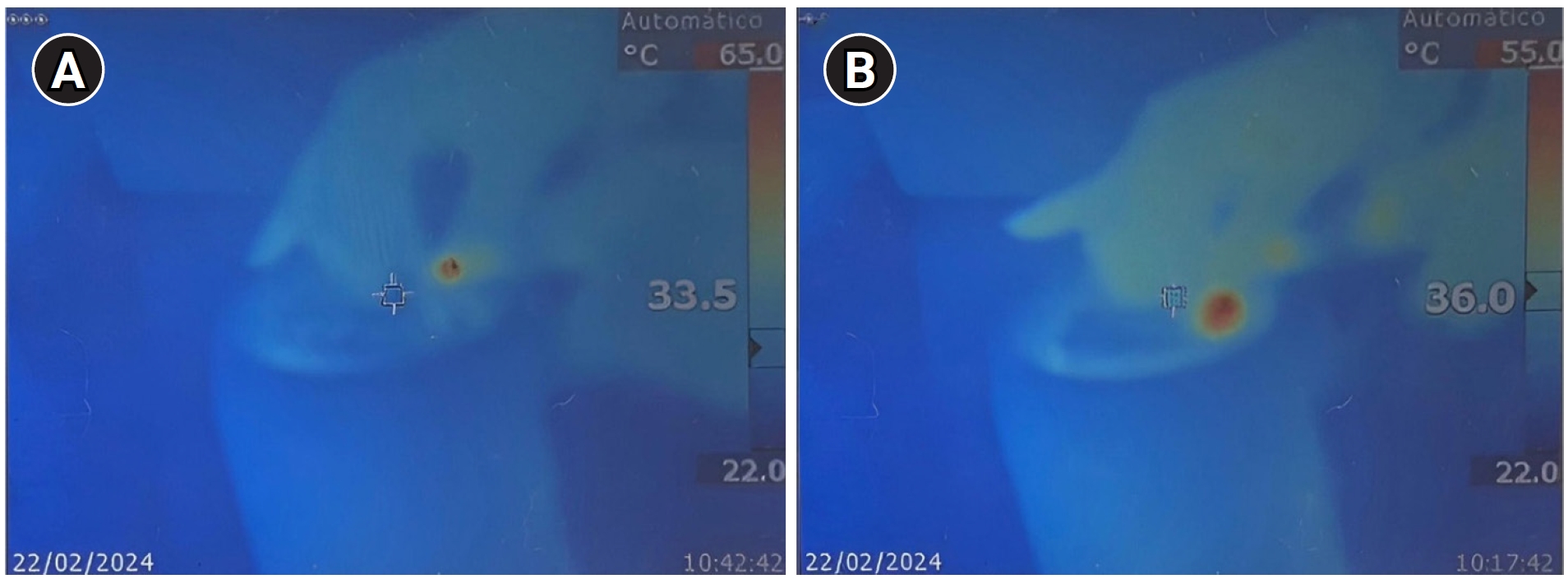
Table 1.Temperature recorded on the tooth’s external surface and the ultrasonic insert at 15, 30, 60, 90, and 120 second intervals in both the adapter-coupled and one-piece insert groups
|
Temperature variation |
Inserts |
Time (sec)
|
|
15 |
30 |
60 |
90 |
120 |
|
Tooth |
Adapter-coupled |
38.6 ± 1.91a,A
|
41.6 ± 3.13a,B
|
44.6 ± 4.26b,C
|
46.5 ± 4.37b,D
|
48.3 ± 4.50b,D
|
|
One-piece |
40.3 ± 3.88a,A
|
45.5 ± 6.23a,B
|
50.0 ± 6.53a,C
|
52.7 ± 7.73a,D
|
55.6 ± 9.06a,E
|
|
Insert |
Adapter-coupled |
44.8 ± 1.96a,A
|
47.5 ± 2.39a,A
|
52.8 ± 5.37a,B
|
56.1 ± 6.91a,C
|
58.5 ± 7.99a,D
|
|
One-piece |
34.6 ± 3.73b,A
|
36.3 ± 5.68b,A
|
42.7 ± 2.90b,B
|
45.1 ± 4.23b,C
|
46.4 ± 4.74b,C
|
REFERENCES
- 1. Dewes Cassal M, Cardoso Soares P, Dos Santos M. The effect of combined ultrasonic tip and mechanized instrumentation on the reduction of the percentage of non-instrumented surfaces in oval/flat root canals: a systematic review and meta-analysis. Cureus 2023;15:e50041.ArticlePubMedPMC
- 2. Crozeta BM, Lopes FC, Menezes Silva R, Silva-Sousa YT, Moretti LF, Sousa-Neto MD. Retreatability of BC Sealer and AH Plus root canal sealers using new supplementary instrumentation protocol during non-surgical endodontic retreatment. Clin Oral Investig 2021;25:891-899.ArticlePubMedPDF
- 3. da Rosa AF, Fischer BV, Dias-Junior LC, Serique AV, Bortoluzzi EA, Teixeira CD, et al. Effectiveness of different supplementary protocols for remaining filling material removal in endodontic reintervention: an integrative review. Odontology 2024;112:51-73.ArticlePubMedPDF
- 4. Ekici Ö, Aslantaş K, Kanık Ö, Keleş A. Evaluation of surface roughness after root resection: an optical profilometer study. Microsc Res Tech 2021;84:828-836.ArticlePubMedPDF
- 5. Neelakantan P, Vishwanath V, Taschieri S, Corbella S. Present status and future directions: minimally invasive root canal preparation and periradicular surgery. Int Endod J 2022;55 Suppl 4:845-871.ArticlePubMedPDF
- 6. Zogheib C, Roumi R, Bourbouze G, Naaman A, Khalil I, Plotino G. Effects of ultrasonic refinement on endodontic access cavity walls: a microcomputed tomography analysis. J Conserv Dent 2021;24:29-35.ArticlePubMedPMC
- 7. Zogheib C, Roumi R, Baldi A, Palopoli P, Pasqualini D, Berutti E, et al. The effect of ultrasonic access cavity preparation on dentinal inner walls: a micro-CT study on cadaveric samples. Oral Radiol 2023;39:639-645.ArticlePubMedPDF
- 8. Görduysus MO, Görduysus M, Friedman S. Operating microscope improves negotiation of second mesiobuccal canals in maxillary molars. J Endod 2001;27:683-686.ArticlePubMed
- 9. Camacho-Aparicio LA, Borges-Yáñez SA, Estrada D, Azcárraga M, Jiménez R, González-Plata-R R. Validity of the dental operating microscope and selective dentin removal with ultrasonic tips for locating the second mesiobuccal canal (MB2) in maxillary first molars: An in vivo study. J Clin Exp Dent 2022;14:e471-e478.ArticlePubMedPMC
- 10. Pietrzycka K, Pawlicka H. Clinical aspects of pulp stones: a case report series. Dent Med Probl 2020;57:213-220.ArticlePubMed
- 11. Arun N, Ramesh S, Sankar A. Knowledge, attitude, and practice of ultrasonics in endodontic treatment: a Survey among general practitioners and endodontists. J Adv Pharm Technol Res 2022;13(Suppl 1):S173-S176.ArticlePubMedPMC
- 12. Terauchi Y, Sexton C, Bakland LK, Bogen G. Factors affecting the removal time of separated instruments. J Endod 2021;47:1245-1252.ArticlePubMed
- 13. Özdayi K, Yilmaz S, Dumani A, Yoldas O. Effects of ultrasonics and trephine burs on dentinal microcrack formation during broken instrument removal procedures: a micro-CT analysis. Aust Endod J 2024;50:123-130.ArticlePubMed
- 14. Serpa GC, Guedes OA, Freitas NS, Silva JA, Estrela C, Decurcio DA. The effect of ultrasonic vibration protocols for cast post removal on the incidence of root dentin defects. J Oral Sci 2023;65:190-194.ArticlePubMed
- 15. Abella Sans F, Alatiya ZT, Val GG, Nagendrababu V, Dummer PM, Durán-Sindreu Terol F, et al. A laboratory study comparing the static navigation technique using a bur with a conventional freehand technique using ultrasonic tips for the removal of fibre posts. Int Endod J 2024;57:355-368.ArticlePubMed
- 16. Rivera-Peña ME, Duarte MA, Alcalde MP, Furlan RD, Só MV, Vivan RR. Ultrasonic tips as an auxiliary method for the instrumentation of oval-shaped root canals. Braz Oral Res 2019;33:e011.ArticlePubMed
- 17. Santos-Junior AO, Tanomaru-Filho M, Pinto JC, Tavares KI, Pivoto-João MM, Guerreiro-Tanomaru JM. New ultrasonic tip decreases uninstrumented surface and debris in flattened canals: a micro-computed tomographic study. J Endod 2020;46:1712-1718.ArticlePubMed
- 18. Boutsioukis C, Arias-Moliz MT. Present status and future directions: irrigants and irrigation methods. Int Endod J 2022;55(Suppl 3):588-612.ArticlePubMedPMCPDF
- 19. Paixão S, Rodrigues C, Grenho L, Fernandes MH. Efficacy of sonic and ultrasonic activation during endodontic treatment: a Meta-analysis of in vitro studies. Acta Odontol Scand 2022;80:588-595.ArticlePubMed
- 20. Kim SY, Jang YE, Kim BS, Pang EK, Shim K, Jin HR, et al. Effects of ultrasonic activation on root canal filling quality of single-cone obturation with calcium silicate-based sealer. Materials (Basel) 2021;14:1292.ArticlePubMedPMC
- 21. Iandolo A, Amato A, Abdellatif D, Pantaleo G, Amato M. Special Issue “The state of the art in endodontics”. J Clin Med 2022;11:2329.ArticlePubMedPMC
- 22. Plotino G, Pameijer CH, Grande NM, Somma F. Ultrasonics in endodontics: a review of the literature. J Endod 2007;33:81-95.ArticlePubMed
- 23. Budd JC, Gekelman D, White JM. Temperature rise of the post and on the root surface during ultrasonic post removal. Int Endod J 2005;38:705-711.ArticlePubMed
- 24. Hashem AA. Ultrasonic vibration: temperature rise on external root surface during broken instrument removal. J Endod 2007;33(9):1070-3; doi: 10.1016/j.joen.2007.06.005.ArticlePubMed
- 25. Madarati AA, Qualtrough AJ, Watts DC. Factors affecting temperature rise on the external root surface during ultrasonic retrieval of intracanal separated files. J Endod 2008;34:1089-1092.ArticlePubMed
- 26. Madarati AA, Qualtrough AJ, Watts DC. Efficiency of a newly designed ultrasonic unit and tips in reducing temperature rise on root surface during the removal of fractured files. J Endod 2009;35:896-899.ArticlePubMed
- 27. Ekici Ö, Aslantaş K, Kanık Ö, Keles A. Temperature and time variations during apical resection. Acta Odontol Scand 2021;79:156-160.ArticlePubMed
- 28. Eriksson AR, Albrektsson T. Temperature threshold levels for heat-induced bone tissue injury: a vital-microscopic study in the rabbit. J Prosthet Dent 1983;50:101-107.ArticlePubMed
- 29. Walters JD, Rawal SY. Severe periodontal damage by an ultrasonic endodontic device: a case report. Dent Traumatol 2007;23:123-127.ArticlePubMed
- 30. Sauk JJ, Norris K, Foster R, Moehring J, Somerman MJ. Expression of heat stress proteins by human periodontal ligament cells. J Oral Pathol 1988;17:496-499.ArticlePubMed
- 31. Line SE, Polson AM, Zander HA. Relationship between periodontal injury, selective cell repopulation and ankylosis. J Periodontol 1974;45:725-730.ArticlePubMed
- 32. Kocher T, Plagmann HC. Heat propagation in dentin during instrumentation with different sonic scaler tips. Quintessence Int 1996;27:259-264.PubMed
- 33. Cameron JA. The effect of ultrasonic endodontics on the temperature of the root canal wall. J Endod 1988;14:554-559.ArticlePubMed
- 34. Shiyakov KK, Vasileva RI. Resonance compatibility between endosonic tips and ultrasonic devices of different brands. J IMAB 2014;20:621-625.Article
 , Bruno Monguilhott Crozeta2
, Bruno Monguilhott Crozeta2 , Bruno Marques-da-Silva1
, Bruno Marques-da-Silva1 , Alysson Nunes Diógenes1
, Alysson Nunes Diógenes1 , Emmanuel João Nogueira Leal da Silva2,3
, Emmanuel João Nogueira Leal da Silva2,3 , Flávia Sens Fagundes Tomazinho1,*
, Flávia Sens Fagundes Tomazinho1,*


 KACD
KACD
 ePub Link
ePub Link Cite
Cite