Articles
- Page Path
- HOME > Restor Dent Endod > Volume 38(2); 2013 > Article
-
Research Article
Inhibition of
Streptococcus mutans biofilm formation on composite resins containing ursolic acid - Soohyeon Kim1, Minju Song1, Byoung-Duck Roh2, Sung-Ho Park2, Jeong-Won Park1
-
2013;38(2):-72.
DOI: https://doi.org/10.5395/rde.2013.38.2.65
Published online: May 28, 2013
1Department of Conservative Dentistry, Gangnam Severance Hospital, Yonsei University College of Dentistry, Seoul, Korea.
2Department of Conservative Dentistry, Yonsei University College of Dentistry, Seoul, Korea.
- Correspondence to Jeong-Won Park, DDS, PhD. Associate Professor, Department of Conservative Dentistry, Yonsei University College of Dentistry, 146-92 Dogok-dong, Gangnam-gu, Seoul, Korea 135-720. TEL, +82-2-2019-1350; FAX, +82-2-3463-4052; pjw@yuhs.ac
©Copyights 2013. The Korean Academy of Conservative Dentistry.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,865 Views
- 5 Download
- 26 Crossref
Abstract
-
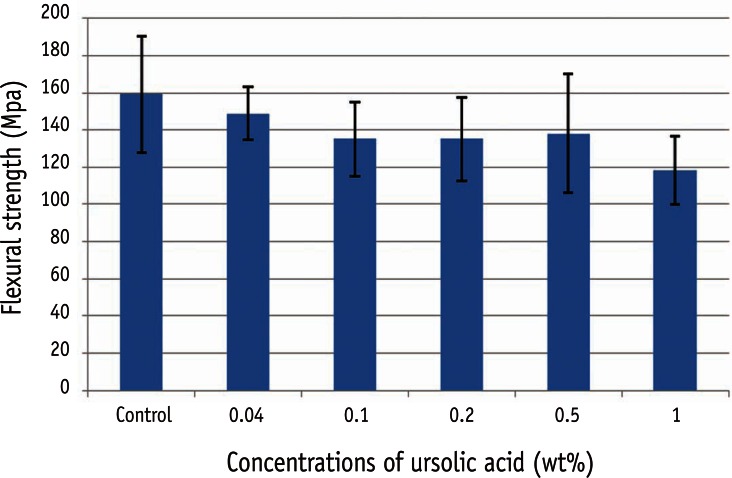
Objectives To evaluate the inhibitory effect of ursolic acid (UA)-containing composites on Streptococcus mutans (S. mutans) biofilm.
-
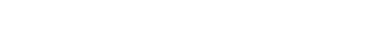
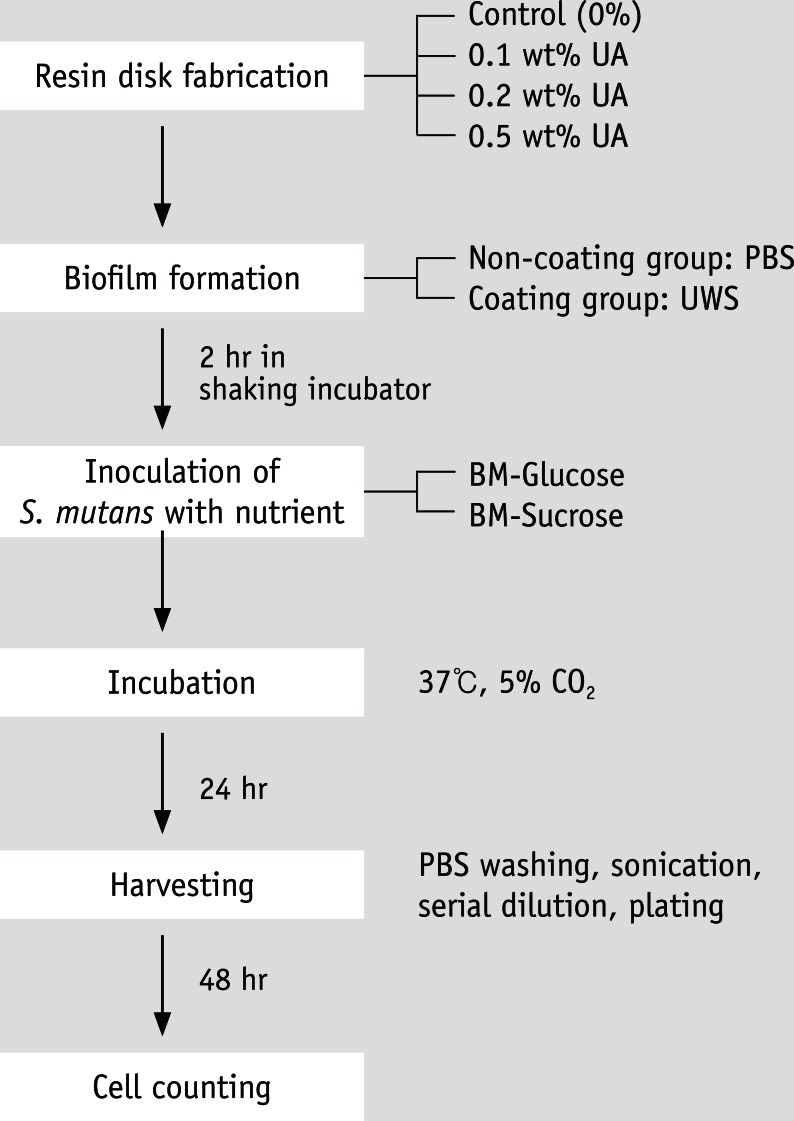
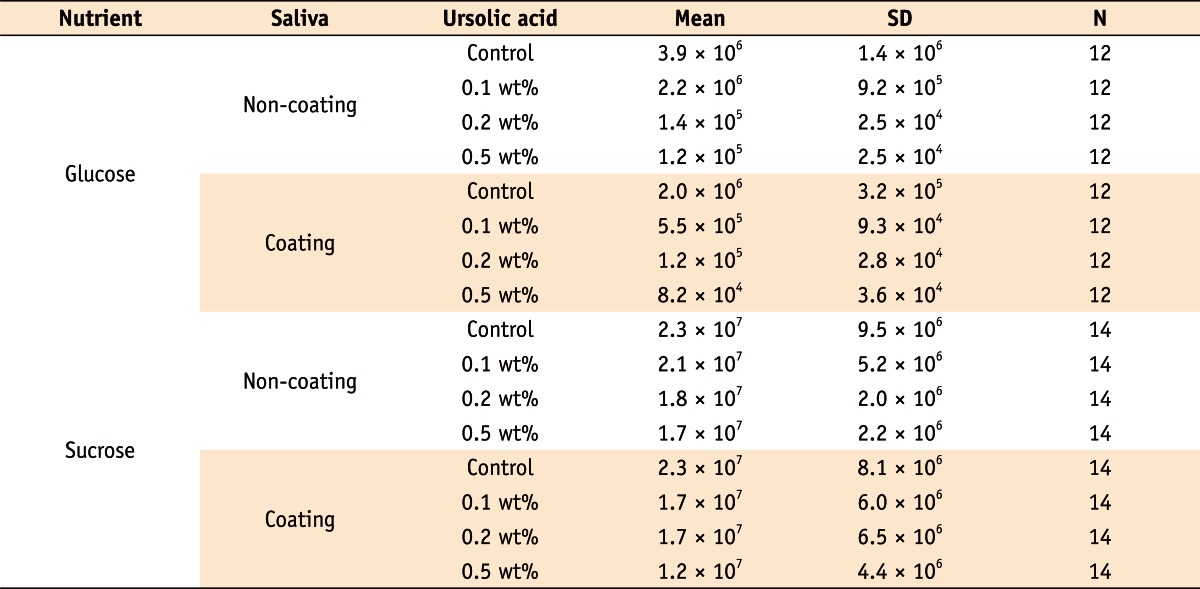
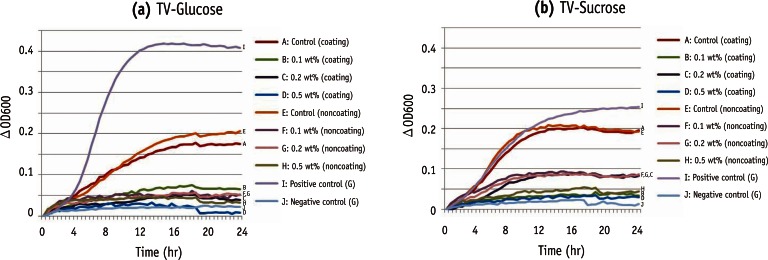
Materials and Methods Composite resins with five different concentrations (0.04, 0.1, 0.2, 0.5, and 1.0 wt%) of UA (U6753, Sigma Aldrich) were prepared, and their flexural strengths were measured according to ISO 4049. To evaluate the effect of carbohydrate source on biofilm formation, either glucose or sucrose was used as a nutrient source, and to investigate the effect of saliva treatment, the specimen were treated with either unstimulated whole saliva or phosphate-buffered saline (PBS). For biofilm assay, composite disks were transferred to S. mutans suspension and incubated for 24 hr. Afterwards, the specimens were rinsed with PBS and sonicated. The colony forming units (CFU) of the disrupted biofilm cultures were enumerated. For growth inhibition test, the composites were placed on a polystyrene well cluster, and S. mutans suspension was inoculated. The optical density at 600 nm (OD600) was recorded by Infinite F200 pro apparatus (TECAN). One-way ANOVA and two-way ANOVA followed by Bonferroni correction were used for the data analyses.
-
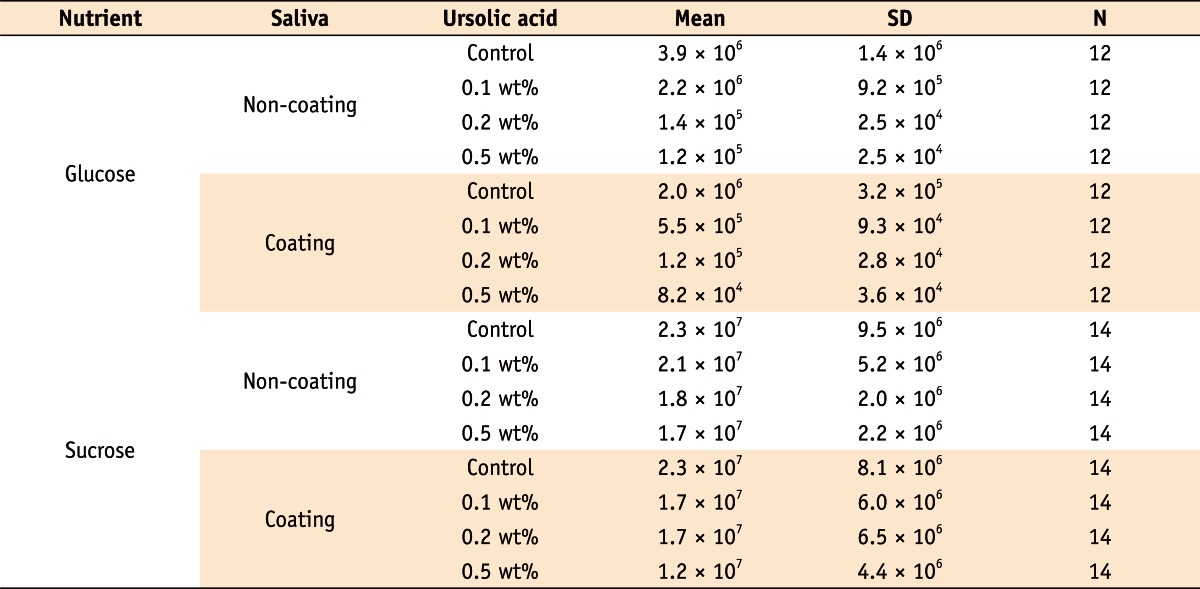
Results The flexural strength values did not show significant difference at any concentration (p > 0.01). In biofilm assay, the CFU score decreased as the concentration of UA increased. The influence of saliva pretreatment was conflicting. The sucrose groups exhibited higher CFU score than glucose group (p < 0.05). In bacterial growth inhibition test, all experimental groups containing UA resulted in complete inhibition.
-
Conclusions Within the limitations of the experiments, UA included in the composite showed inhibitory effect on S. mutans biofilm formation and growth.
Introduction
Materials and Methods
Results
Discussion
Conclusions
-
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A091074).
-
No potential conflict of interest relevant to this article was reported.
- 1. Haj-Ali R, Walker MP, Williams K. Survey of general dentists regarding posterior restorations, selection criteria, and associated clinical problems. Gen Dent 2005;53:369-375.PubMed
- 2. Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater 2007;23:2-8.ArticlePubMed
- 3. Beyth N, Yudovin-Farber I, Bahir R, Domb AJ, Weiss EI. Antibacterial activity of dental composites containing quaternary ammonium polyethylenimine nanoparticles against Streptococcus mutans. Biomaterials 2006;27:3995-4002.ArticlePubMed
- 4. Leung D, Spratt DA, Pratten J, Gulabivala K, Mordan NJ, Young AM. Chlorhexidine-releasing methacrylate dental composite materials. Biomaterials 2005;26:7145-7153.ArticlePubMed
- 5. Stobie N, Duffy B, McCormack DE, Colreavy J, Hidalgo M, McHale P, Hinder SJ. Prevention of Staphylococcus epidermidis biofilm formation using a low-temperature processed silver-doped phenyltriethoxysilane sol-gel coating. Biomaterials 2008;29:963-969.ArticlePubMed
- 6. Imazato S, Kinomoto Y, Tarumi H, Torii M, Russell RR, McCabe JF. Incorporation of antibacterial monomer MDPB into dentin primer. J Dent Res 1997;76:768-772.ArticlePubMedPDF
- 7. Fan C, Chu L, Rawls HR, Norling BK, Cardenas HL, Whang K. Development of an antimicrobial resin-a pilot study. Dent Mater 2011;27:322-328.ArticlePubMed
- 8. Nohr RS, Macdonald JG. New biomaterials through surface segregation phenomenon: new quaternary ammonium compounds as antibacterial agents. J Biomater Sci Polym Ed 1994;5:607-619.ArticlePubMed
- 9. Liu J. Oleanolic acid and ursolic acid: research perspectives. J Ethnopharmacol 2005;100:92-94.ArticlePubMed
- 10. Liu J. Pharmacology of oleanolic acid and ursolic acid. J Ethnopharmacol 1995;49:57-68.ArticlePubMed
- 11. Fontanay S, Grare M, Mayer J, Finance C, Duval RE. Ursolic, oleanolic and betulinic acids: antibacterial spectra and selectivity indexes. J Ethnopharmacol 2008;120:272-276.ArticlePubMed
- 12. Takahashi N, Nyvad B. The role of bacteria in the caries process: ecological perspectives. J Dent Res 2011;90:294-303.ArticlePubMedPDF
- 13. Costerton JW, Lewandowski Z, DeBeer D, Caldwell D, Korber D, James G. Biofilms, the customized microniche. J Bacteriol 1994;176:2137-2142.ArticlePubMedPMCPDF
- 14. Shapiro S, Giertsen E, Guggenheim B. An in vitro oral biofilm model for comparing the efficacy of antimicrobial mouthrinses. Caries Res 2002;36:93-100.ArticlePubMedPDF
- 15. Hardt M, Witkowska HE, Webb S, Thomas LR, Dixon SE, Hall SC, Fisher SJ. Assessing the effects of diurnal variation on the composition of human parotid saliva: quantitative analysis of native peptides using iTRAQ reagents. Anal Chem 2005;77:4947-4954.ArticlePubMed
- 16. Allaker RP, Douglas CW. Novel anti-microbial therapies for dental plaque-related diseases. Int J Antimicrob Agents 2009;33:8-13.ArticlePubMed
- 17. Jeon JG, Rosalen PL, Falsetta ML, Koo H. Natural products in caries research: current (limited) knowledge, challenges and future perspective. Caries Res 2011;45:243-263.ArticlePubMedPMCPDF
- 18. Kim MJ, Kim CS, Park JY, Lim YK, Park SN, Ahn SJ, Jin DC, Kim TH, Kook JK. Antimicrobial effects of ursolic acid against mutans streptococci isolated from Koreans. Int J Oral Biol 2011;36:7-11.
- 19. Cowan MM. Plant products as antimicrobial agents. Clin Microbiol Rev 1999;12:564-582.ArticlePubMedPMCPDF
- 20. Kurek A, Grudniak AM, Szwed M, Klicka A, Samluk L, Wolska KI, Janiszowska W, Popowska M. Oleanolic acid and ursolic acid affect peptidoglycan metabolism in Listeria monocytogenes. Antonie Van Leeuwenhoek 2010;97:61-68.ArticlePubMedPDF
- 21. Kohda H, Kozai K, Nagasaka N, Miyake Y, Suginaka H, Hidaka K, Yamasaki K. Prevention of dental caries by Oriental folk medicines-active principles of Zizyphi Fructus for inhibition of insoluble glucan formation by cariogenic bacterium Streptococcus mutans. Planta Med 1986;(2):119-120.ArticlePubMed
- 22. Ooshima T, Matsumura M, Hoshino T, Kawabata S, Sobue S, Fujiwara T. Contributions of three glycosyltransferases to sucrose-dependent adherence of Streptococcus mutans. J Dent Res 2001;80:1672-1677.ArticlePubMedPDF
- 23. Gibbons RJ. Role of adhesion in microbial colonization of host tissues: a contribution of oral microbiology. J Dent Res 1996;75:866-870.ArticlePubMedPDF
- 24. Cross SE, Kreth J, Zhu L, Sullivan R, Shi W, Qi F, Gimzewski JK. Nanomechanical properties of glucans and associated cell-surface adhesion of Streptococcus mutans probed by atomic force microscopy under in situ conditions. Microbiology 2007;153:3124-3132.ArticlePubMed
- 25. Schilling KM, Bowen WH. Glucans synthesized in situ in experimental salivary pellicle function as specific binding sites for Streptococcus mutans. Infect Immun 1992;60:284-295.ArticlePubMedPMCPDF
- 26. Ren D, Zuo R, González Barrios AF, Bedzyk LA, Eldridge GR, Pasmore ME, Wood TK. Differential gene expression for investigation of Escherichia coli biofilm inhibition by plant extract ursolic acid. Appl Environ Microbiol 2005;71:4022-4034.ArticlePubMedPMCPDF
REFERENCES


Tables & Figures
REFERENCES
Citations

- Environmental Stress Induces Altered Composition of Streptococcus mutans Membrane Vesicles: pH‐Driven Changes in Membrane Vesicle Production and Composition
Taylor C. Boone, Swetha K. Shankar, Melodie L. Weller
Molecular Oral Microbiology.2026;[Epub] CrossRef - Anti-cariogenic effect of experimental resin cement containing ursolic acid using dental microcosm biofilm
Jonghyun Jo, Mi-Jeong Jeon, Sun Kyu Park, Su-Jung Shin, Baek-il Kim, Jeong-Won Park
Journal of Dentistry.2024; 151: 105447. CrossRef - Rapid specific detection of oral bacteria using Cas13-based SHERLOCK
Jett Liu, Camden Carmichael, Hatice Hasturk, Wenyuan Shi, Batbileg Bor
Journal of Oral Microbiology.2023;[Epub] CrossRef - Novel Bioactive Nanocomposites Containing Calcium Fluoride and Calcium Phosphate with Antibacterial and Low-Shrinkage-Stress Capabilities to Inhibit Dental Caries
Abdullah Alhussein, Rashed Alsahafi, Abdulrahman A. Balhaddad, Lamia Mokeem, Abraham Schneider, Mary-Ann Jabra-Rizk, Radi Masri, Gary D. Hack, Thomas W. Oates, Jirun Sun, Michael D. Weir, Hockin H. K. Xu
Bioengineering.2023; 10(9): 991. CrossRef - Quorum sensing inhibition and antibiofilm action of triterpenoids: An updated insight
Sudipta Paul Bhattacharya, Snigdha Karmakar, Kusumita Acharya, Arijit Bhattacharya
Fitoterapia.2023; 167: 105508. CrossRef - The Application of Small Molecules to the Control of Typical Species Associated With Oral Infectious Diseases
Sirui Yang, Xiaoying Lyu, Jin Zhang, Yusen Shui, Ran Yang, Xin Xu
Frontiers in Cellular and Infection Microbiology.2022;[Epub] CrossRef - Anti-Planktonic and Anti-Biofilm Properties of Pentacyclic Triterpenes—Asiatic Acid and Ursolic Acid as Promising Antibacterial Future Pharmaceuticals
Zuzanna Sycz, Dorota Tichaczek-Goska, Dorota Wojnicz
Biomolecules.2022; 12(1): 98. CrossRef - Development and Physicochemical Characterization of Eugenia brejoensis Essential Oil-Doped Dental Adhesives with Antimicrobial Action towards Streptococcus mutans
Maury Luz Pereira, Danyelle Cristina Pereira Santos, Carlos Alberto Mendes Soares Júnior, Tamyris Alicely Xavier Nogueira Bazan, Clovis Macêdo Bezerra Filho, Márcia Vanusa da Silva, Maria Tereza dos Santos Correia, Andres Felipe Millan Cardenas, Fabiana S
Journal of Functional Biomaterials.2022; 13(3): 149. CrossRef - Does Secondary Plant Metabolite Ursolic Acid Exhibit Antibacterial Activity against Uropathogenic Escherichia coli Living in Single- and Multispecies Biofilms?
Zuzanna Sycz, Dorota Wojnicz, Dorota Tichaczek-Goska
Pharmaceutics.2022; 14(8): 1691. CrossRef - Prolonged Inhibition of Streptococcus mutans Growth and Biofilm Formation by Sustained Release of Chlorhexidine from Varnish Coated Dental Abutments: An in Vitro Study
Mark Feldman, Walid Shaaban Moustafa Elsayed, Michael Friedman, Irith Gati, Doron Steinberg, Hesham Marei, Paolo Francesco Manicone
International Journal of Dentistry.2022;[Epub] CrossRef - Interkingdom Signaling Interference: The Effect of Plant-Derived Small Molecules on Quorum Sensing in Plant-Pathogenic Bacteria
Janak Raj Joshi, Netaly Khazanov, Amy Charkowski, Adi Faigenboim, Hanoch Senderowitz, Iris Yedidia
Annual Review of Phytopathology.2021; 59(1): 153. CrossRef - Small Molecule Compounds, A Novel Strategy against Streptococcus mutans
Sirui Yang, Jin Zhang, Ran Yang, Xin Xu
Pathogens.2021; 10(12): 1540. CrossRef - Titanium dioxide nanotubes added to glass ionomer cements affect S. mutans viability and mechanisms of virulence
Isaac Jordão de Souza ARAÚJO, Mariana Gallante RICARDO, Orisson Ponce GOMES, Priscila Alves GIOVANI, Júlia PUPPIN-RONTANI, Vanessa Arias PECORARI, Elizabeth Ferreira MARTINEZ, Marcelo Henrique NAPIMOGA, Francisco Humberto NOCITI JUNIOR, Regina Maria PUPPI
Brazilian Oral Research.2021;[Epub] CrossRef - Effect of Ursolic and Oleanolic Acids on Lipid Membranes: Studies on MRSA and Models of Membranes
Sandrine Verstraeten, Lucy Catteau, Laila Boukricha, Joelle Quetin-Leclercq, Marie-Paule Mingeot-Leclercq
Antibiotics.2021; 10(11): 1381. CrossRef - Ursolic acid inhibits multi-species biofilms developed by Streptococcus mutans, Streptococcus sanguinis, and Streptococcus gordonii
Xiaoying Lyu, Liang Wang, Yusen Shui, Qingsong Jiang, Lan Chen, Wen Yang, Xiaoya He, Jumei Zeng, Yuqing Li
Archives of Oral Biology.2021; 125: 105107. CrossRef - The physical properties and anticariogenic effect of experimental resin cement containing ursolic acid
Hyunkyung Yoo, So Youn Kim, Su-Jung Shin, Jeong-Won Park
Odontology.2021; 109(3): 641. CrossRef - Ursolic acid: A systematic review of its pharmacology, toxicity and rethink on its pharmacokinetics based on PK-PD model
Qiang Sun, Man He, Meng Zhang, Sha Zeng, Li Chen, Lijuan Zhou, Haibo Xu
Fitoterapia.2020; 147: 104735. CrossRef - Effects of UVB and UVC irradiation on cariogenic bacteria in vitro
Shigeki Uchinuma, Yasushi Shimada, Khairul Matin, Keiichi Hosaka, Masahiro Yoshiyama, Yasunori Sumi, Junji Tagami
Lasers in Medical Science.2019; 34(5): 981. CrossRef - Ursolic acid (UA): A metabolite with promising therapeutic potential
Dharambir Kashyap, Hardeep Singh Tuli, Anil K. Sharma
Life Sciences.2016; 146: 201. CrossRef - Protective Effects on Gastric Lesion of Ursolic acid
Sun Whoe Kim, In Young Hwang, Sun Yi Lee, Choon Sik Jeong
Journal of Food Hygiene and Safety.2016; 31(4): 286. CrossRef - Ursolic Acid—A Pentacyclic Triterpenoid with a Wide Spectrum of Pharmacological Activities
Łukasz Woźniak, Sylwia Skąpska, Krystian Marszałek
Molecules.2015; 20(11): 20614. CrossRef - Antibacterial effect of self-etching adhesive systems onStreptococcus mutans
Seung-Ryong Kim, Dong-Hoon Shin
Restorative Dentistry & Endodontics.2014; 39(1): 32. CrossRef - Dental materials with antibiofilm properties
Zhejun Wang, Ya Shen, Markus Haapasalo
Dental Materials.2014; 30(2): e1. CrossRef - Antibacterial properties of composite resins incorporating silver and zinc oxide nanoparticles onStreptococcus mutansandLactobacillus
Shahin Kasraei, Lida Sami, Sareh Hendi, Mohammad-Yousef AliKhani, Loghman Rezaei-Soufi, Zahra Khamverdi
Restorative Dentistry & Endodontics.2014; 39(2): 109. CrossRef - Synergistic effect of xylitol and ursolic acid combination on oral biofilms
Yunyun Zou, Yoon Lee, Jinyoung Huh, Jeong-Won Park
Restorative Dentistry & Endodontics.2014; 39(4): 288. CrossRef - The virulence of Streptococcus mutans and the ability to form biofilms
W. Krzyściak, A. Jurczak, D. Kościelniak, B. Bystrowska, A. Skalniak
European Journal of Clinical Microbiology & Infectious Diseases.2014; 33(4): 499. CrossRef
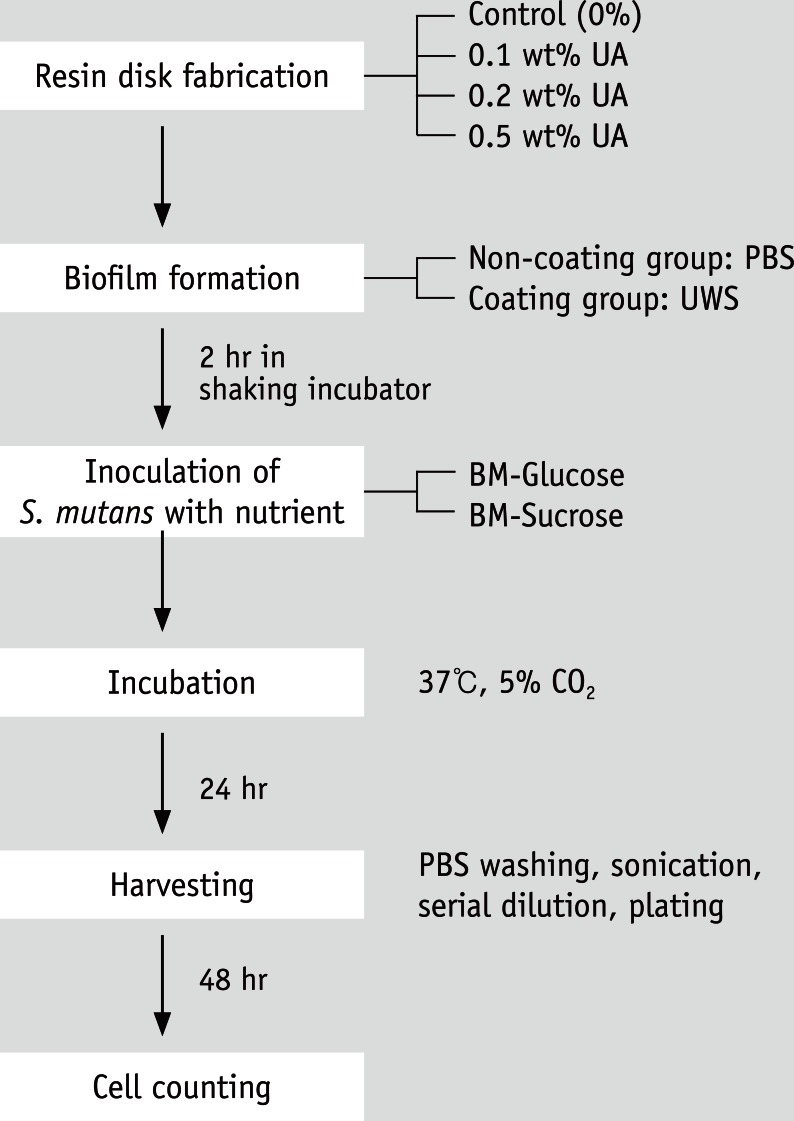
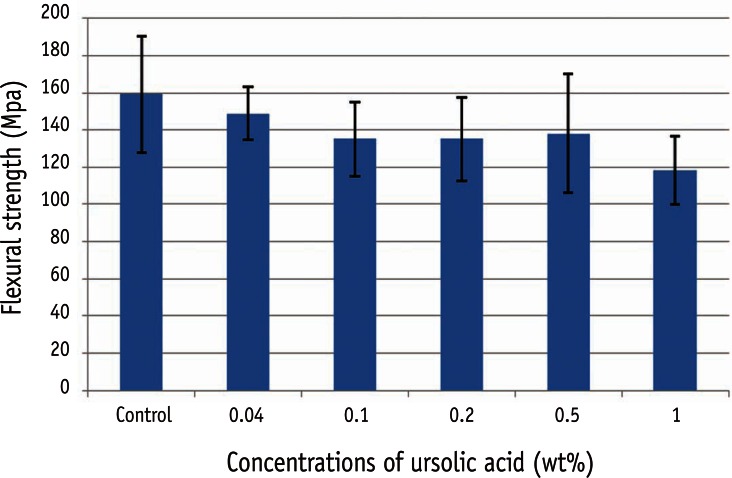
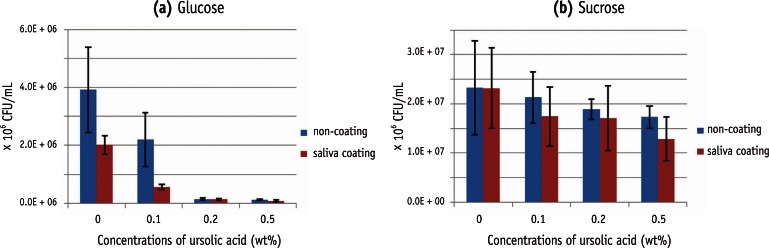
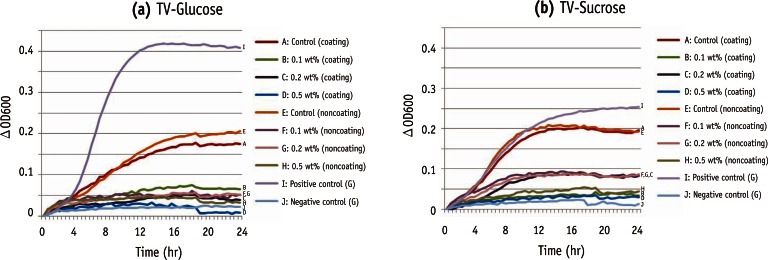
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
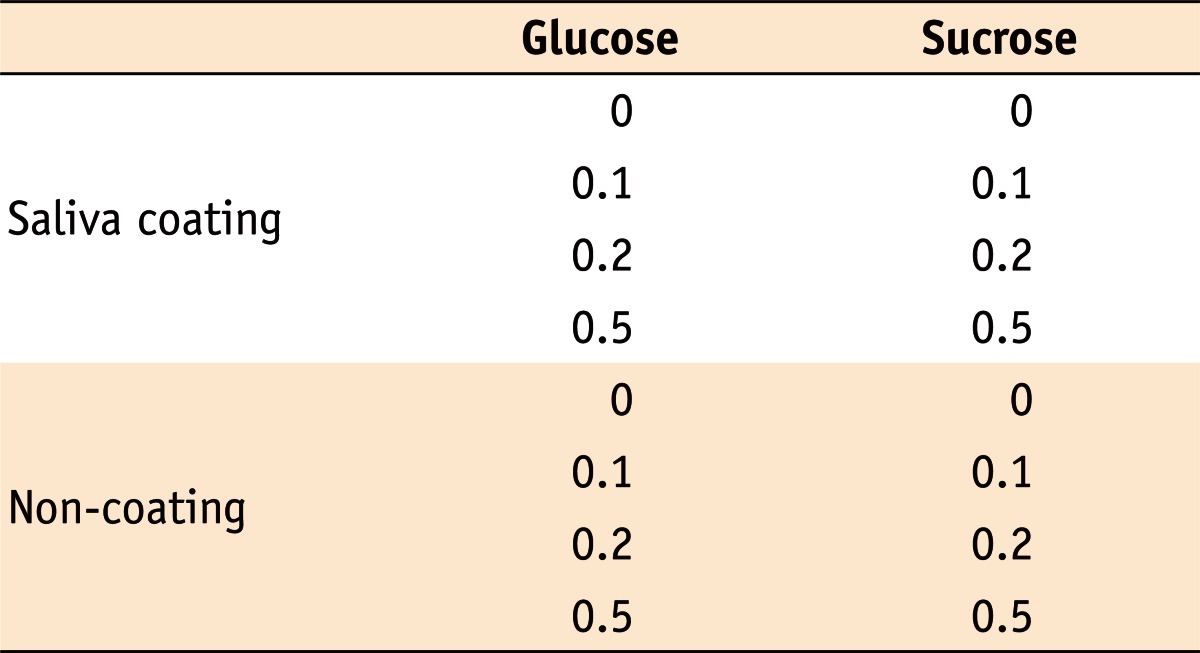
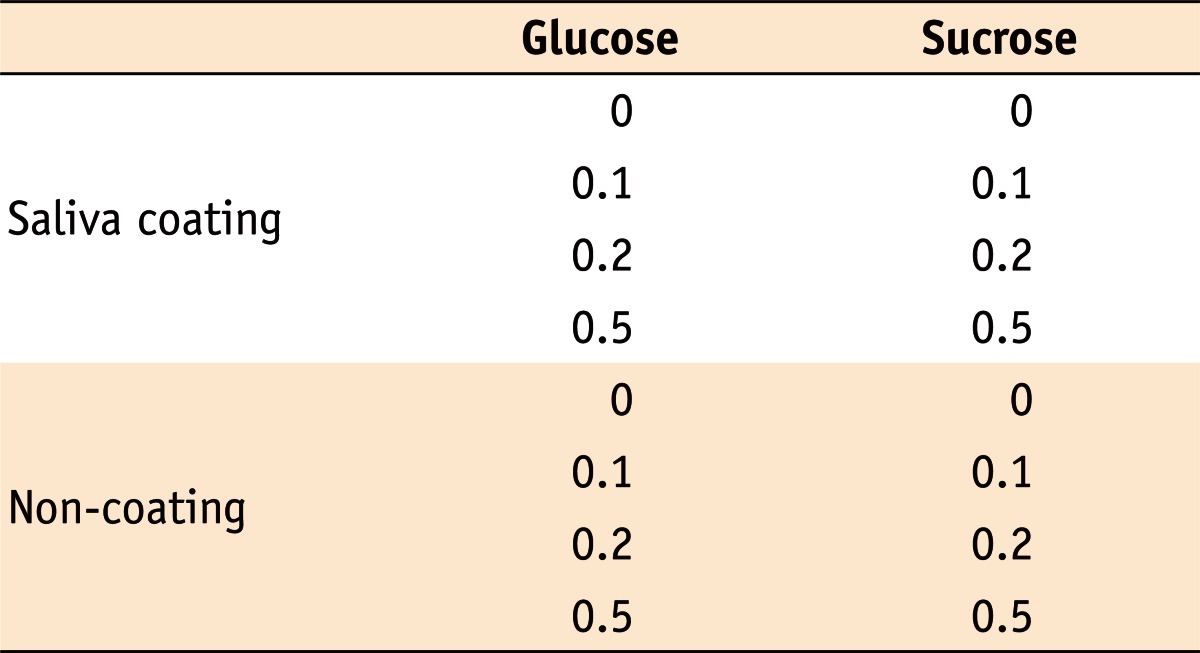
Ursolic acid concentrations (%) for each experimental condition
Colony forming unit of Streptococcus mutans in biofilm assay (CFU/mL)

 KACD
KACD
 ePub Link
ePub Link Cite
Cite